What is deep brain stimulation?
Deep brain stimulation (DBS) is a treatment option for certain conditions that involves surgery to place electrodes within a specific area of the brain. The electrodes are then used to deliver an electrical current to relieve neurological symptoms associated with conditions such as epilepsy or movement disorders.
DBS is used to treat a condition when other treatments, such as medications or special diets, do not work to relieve symptoms or if the treatments produce unwanted side effects. In adults, DBS is most commonly used to treat Parkinson’s disease and tremor. In children, DBS has been most commonly used to treat dystonia, chorea and epilepsy. DBS is not a cure for any of these conditions but can be an effective treatment to relieve symptoms and improve quality of life.
How does deep brain stimulation work?
Implantation of the DBS system is a surgical procedure which is done by a neurosurgeon while your child is under general anaesthesia. The front of your child’s hair is shaved and an incision approximately 5 inches (12.7cm) long is made behind the hairline. The neurosurgeon then places thin wires into a specific target in the brain. These wires are then tunneled under the skin and connected to an internal pulse generator (IPG). The IPG is like a battery which is placed under the skin in the chest area similar to a pacemaker.
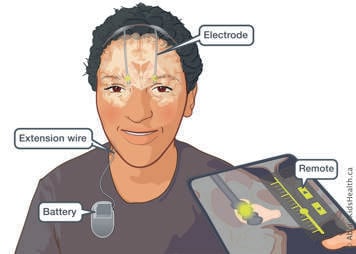
The different parts of the DBS system are explained below.
Electrodes
- Very thin wires are placed deep inside your child’s brain.
- The tip of each electrode is positioned in the specific part of the brain that is the source of a particular symptom.
- The target area of the brain will depend on the symptoms being treated.
Extension wires
- Wires are placed under the skin of the scalp, neck and chest.
- These wires connect the electrodes to the internal pulse generator (IPG).
Internal pulse generator (IPG) or neurostimulator
- A battery device is implanted under the skin in the chest, near the collarbone.
- This battery can be rechargeable or non rechargeable.
After 4-6 weeks, when your child is home and recovered from the procedure, they will return to clinic to start the process of having the device programmed. This means adjusting the electrical impulses to the setting that best relieves the symptoms with as few side effects as possible.
What are the target areas for deep brain stimulation to treat dystonia and chorea?
The most common target for dystonia or chorea treatment is a deep area in the brain called the globus pallidus pars interna (GPI). GPI plays an important role in movement control and coordination. By delivering a gentle electric current to the GPI, DBS can decrease dystonic movements, including repetitive or twisting movements.
Through a careful process the DBS system will be programmed to help your child have the most benefit from stimulation and minimize unwanted side effects. The potential side effects that can be seen with stimulation of GPI include problems with speaking, swallowing and walking. All these symptoms are reversible with adjusting the stimulation settings.
What are the target areas for deep brain stimulation to treat epilepsy?
The most common target for epilepsy treatment is a deep structure in the brain called the thalamus. The thalamus is important in motor and sensory functions. The DBS team might choose different areas within the thalamus to control your child’s seizures (such as centromedian nucleus or anterior nucleus). This decision depends on the type of epilepsy that your child has.
The main side effects that can be seen from stimulation of the thalamus include depression and problems with memory. All of these symptoms are reversible with adjusting the stimulation settings.
Other targets for specific conditions such as repetitive self-harm are being researched at the Hospital for Sick Children.
Risks from the deep brain stimulation surgery
DBS surgery is generally very safe, but it does have similar risks to other types of brain surgery. While these risks are rare, they are serious, and it is important for you to be aware of them while deciding about surgery. The specific risks of DBS surgery will be discussed with you by your child’s health-care team with reference to your child’s specific health needs.
Deciding if deep brain stimulation is right for your child
Every child and family are unique, and DBS may or may not be the best choice depending on your child’s needs and your family. Your child’s health-care team will help you make an individualized decision about whether DBS is a good option for your child. To gather the information needed to make this decision, your child will have screening assessment appointments to meet with the DBS team.
Who is part of your child’s health-care team?
Neurologists
The neurology team will perform a detailed neurologic exam at your child’s clinic visits. They will also monitor and adjust the stimulation settings after the surgery and teach you about how to manage the DBS remote. The neurologists will communicate with your child’s other physicians to help manage medications.
Neurosurgeons
The neurosurgery team will follow the recommendations from the whole team and perform the surgery if indicated. They will monitor your child’s incision after surgery. Your child’s neurosurgeon will change the IPG when appropriate.
Nursing
The nursing team is essential to the communication around your child’s health. A nurse practitioner may be your initial point of contact for coordinating tests, providing advice and supporting you and your child throughout the whole process.
Psychology
The psychology team may provide a detailed neuro-psychology assessment prior to the DBS surgery. They may also perform tests following surgery to assess if there are psychological effects from stimulation.
Social worker
You and your child may be referred to a social worker to help you cope with emotional, financial and practical issues associated with illness, treatment or long stays at the hospital.
What can I expect from my child’s first clinic visit?
The initial visit is an opportunity for the health-care team to learn about your child and to begin the discussion about whether DBS may be helpful to manage their symptoms. During this visit a detailed medical history will be taken and physical examination will be performed. This first visit can be between 2-3 hours as many members of the team will meet with you and your child.
Videos may be taken to record and document parts of the assessment. These are stored on a private and secure internal hospital server and will help the team monitor progression and response to treatment over time. Once the initial evaluations have been completed you will have the opportunity to ask any questions that you may have about your child’s condition and about DBS.
If surgery is recommended, what other assessments are needed?
MRI of the brain
A magnetic resonance imaging (MRI) appointment will be made if a recent MRI is not available. This MRI is necessary to help evaluate the brain structures and make the best decisions about treatment and electrode placement. Sedation may be given to help your child lie still for the scans. If your child has a vagus nerve stimulator (VNS), it should be turned off for the MRI and turned back on afterwards.
Neuropsychology assessment
During this visit, the neuropsychiatrist will assess your child’s cognition and mental health and the risk of developing problems such as depression or anxiety after DBS surgery. The neuropsychologist will tell you if your child is at risk and may provide recommendations for how to prevent or manage these risks.
Nursing assessment
A nurse from the same-day admissions unit will meet with you and provide you with all the details about how to prepare for surgery and information about what to expect during your hospital stay.
Pre-anaesthesia clinic
You will be given an appointment to meet with anaesthesiologists to assess your child’s safety for general anaesthesia. Your child may have tests, such as blood tests, an electrocardiogram (ECG) and a chest X-ray. Please bring a list of all the medicines taken by your child.
What happens on the day of the surgery?
Before surgery
After you arrive at the hospital and check in, the nurses will help your child get ready for surgery. They will check your child’s blood pressure, pulse and temperature and will provide hospital clothing. You will meet the anaesthesiologist and surgical team.
During surgery
The procedure to implant a DBS system involves multiple steps, all of which will take place on the same day while your child is under anaesthesia. When everything is ready, your child will be taken to the operating room. The anaesthesiologist will provide medications to relax your child and begin the general anaesthesia. A breathing tube will also be inserted.
A frame will the be applied to your child's head. This frame is like a ruler which helps the surgical team measure the most accurate possible placement of the DBS electrodes. Your child will be asleep through this process and will not experience any pain. They will then undergo a head computed tomography (CT) scan. After the CT scan, your child will be brought back to the operating room.
Placing the electrodes
The neurosurgeon will:
- Wash the head with a special soap that kills germs and shave a small amount of hair.
- Make an incision (cut) on to the top of the head and two small round openings in the skull (about the size of a nickel).
- Insert each electrode into the brain using image guidance to ensure that the tip is in the proper target area.
- Stimulate the electrodes and measure how your child’s brain cells react.
- Use plastic caps to close the holes and make sure the electrodes stay in place. The incision is closed with dissolvable sutures.
- Remove the frame from the head.
Placing the extension wires and IPG
Once the electrodes have been placed in the brain, the neurosurgeon will:
- Connect the electrodes in the head to extension wires that will then be tunnelled under your child’s skin, from the top of the head, behind the ear, down the neck to the chest.
- Connect the extension wire to the IPG unit.
- Implant the IPG under the skin below the collarbone. The IPG will remain turned off.
- Close the incision in your child’s chest with dissolvable sutures.
MRI to check electrode placement
Your child will have an MRI immediately after the IPG placement to confirm the location of the electrodes and to make sure there were no unexpected complications. This will be under the same general anaesthesia. After the MRI is complete, your child will return to the operating room where they will be woken up from anaesthesia and the breathing tube will be removed.
After DBS surgery
When the surgery is finished, your child will go the Post Anesthetic Care Unit (PACU) for 1 to 3 hours to recover. The nurses will monitor your child in the PACU and treat any immediate pain.
Your child’s neurosurgeon will meet you and discuss the surgery.
When you see your child, there will be a bandage covering the incision on their head and another bandage over the IPG site.
When your child is ready, they will be brought to the neurosurgery unit. The health-care team will continue to check your child’s condition and progress. In the evening, once they are feeling up to it, your child can start to drink and eat.
In the days following surgery your child may have symptoms such as pain or nausea which can be managed with medications if needed.
Your child will be given a course of antibiotics to decrease the risk of infection. This will be given by IV at first and then will be continued by mouth or feeding tube after discharge home.
Going home after DBS surgery
Your child can expect to go home 3 to 5 days after surgery once they are feeling well enough. Before you leave the hospital, the health-care team will tell you:
- how to take care of your child’s incisions
- when the DBS system will be turned on
- about future follow-up appointments
Recovering at home
At home, your child’s medications will stay the same as they were at the hospital until their DBS system is turned on.
In the weeks following surgery, your child may feel a temporary improvement in their symptoms, even though the DBS system is not yet turned on. This is due to swelling caused by the electrodes. As the swelling goes away, their symptoms will likely return to their baseline (the same as before surgery).
To maximize recovery and minimize the chance of complications, it is important that your child avoid certain activities such as sports and roller coasters for a few months after surgery. It is also important to avoid swimming or submerging the incisions under water for several weeks. Your child’s health-care team will help you decide when it may be safe to resume some of these activities.
Always carry your child’s DBS Registration Card
Before you leave the hospital, your child will get a temporary registration card for their DBS system from the company that makes it. You will receive a permanent card in the mail that your child must always carry with them.
Tell all your child’s health-care providers that they have a DBS system
All your child’s health-care providers need to know that your child has a DBS system implanted in their body so they can take steps to keep your child safe.
Consider getting a MedicAlert bracelet for your child. In an emergency, the bracelet tells health-care professionals who do not know your child that your child has a DBS system.
NEVER apply heat to your DBS system
Do not put heat (i.e. a heating pack, heat source during surgery) on any part of your DBS system as this could damage it and harm your child.
Your child should not have diathermy treatments (heat therapy), which deliver energy to heat and heal tissues in your body. Some common surgeries may use this technique, so it is very important to notify the health-care team in advance that your child has a DBS system.
Check with your child’s doctors before an MRI
Whether it is safe to have an MRI of the brain or body depends on the type of DBS system your child has and the MRI services (in general, the DBS inserted at SickKids is compatible with brain MRI). Performing MRI images of other areas of your child’s body requires consultation with the DBS and MRI safety team and might not be possible.
Check with your child’s doctor or the manufacturer of the device before having other medical procedures
Most medical procedures (such as a CT scan, X-rays, most dental procedures) are safe for children with a DBS system, but some need extra precautions. Other procedures are not possible because they could cause serious harm or death.
Complications from deep brain stimulation surgery
Although many precautions are taken before, during and after surgery to minimize the risk, infection of the DBS hardware is possible. Below is a list of symptoms that may indicate infection. If you notice any of these signs or symptoms, please contact your child’s neurosurgeon or nurse practitioner as soon as possible:
- Redness or swelling at the incision site that is getting worse
- Leaking (for example with yellow or green-like pus) from the incision site
- Bleeding from the incision
- Pain at the incision site that does not go away
- Fever (temperature over 38 °C or 100.4 °F)
There may also be side effects after starting stimulation. At the first programming session, you will hear from your child’s neurology team about the specific side effects of stimulation at your child’s deep brain target. Some commonly seen side effects include visual changes, changes to the voice, muscle contractions and numbness. These side effects are reversible by changing or turning off the stimulation.
Taking care of your child at home after deep brain stimulation surgery
Your child’s incisions will have dissolvable sutures and will be covered with bandages. The bandages will be removed before your child leaves the hospital. The sites can be left without a dressing. You will be given detailed instructions of how to care for the incisions to best facilitate healing before your child leaves the hospital. In general, you should:
- Clean the incisions regularly with soap and water
- Keep your child’s head covered by wearing a scarf or a loose-fitting hat if you bring your child outside
- Never scratch or apply any pressure to the incision sites
Hygiene
- Wash hands frequently.
- Your child can take a shower and have their hair washed with mild soap or shampoo 2-3 days after surgery.
- It is important to clean the incisions but do not submerge them in water for approximately 6 weeks after surgery. This means your child cannot soak in a bathtub or go swimming until fully healed. They should also avoid hot tubs, saunas, and steam rooms during this period.
- Make sure hats, bed linen and pillows are clean.
- Stop pets from going close to the incisions and wash hands well after touching pets.
- Do not use a hair dryer or products such as gel or hairspray until after you see the neurosurgeon in follow-up clinic.
Charging the battery
- Some batteries are rechargeable and can last longer before requiring a replacement surgery.
- If your child has a rechargeable battery, you must recharge it regularly (every day for to 20-30 minutes or every week for 1-2 hours). You don’t need to charge the battery before the first clinic visit.
- At the first programming follow-up, you will get careful and detailed instructions for charging.
- Please bring your child’s kit including charger and remote to every DBS clinic appointment.
Neurosurgery follow-up
You will see your child’s neurosurgeon approximately 4-6 weeks after surgery. They will assess your child’s symptoms and the incision sites. They will give you new instructions about bathing and activity.
Programming your child’s DBS
Your child’s DBS system will be off for several weeks following surgery. Once it is turned on, it will deliver stimulation to the target area of your child’s brain.
Programming is the adjustment of the electrical impulses from the IPG. This occurs approximately 4-6 weeks after surgery when your child’s brain has recovered completely from surgery.
The first programming appointment will take 2 to 3 hours. During this visit, the health-care team will test your child’s response to stimulation and record what levels of stimulation cause side effects.
Your child will need between 4 to 6 more visits to program the stimulator to the best setting. Getting to the best setting can take as long as 6 to 12 months.
The health-care team will give you a remote control to check that the stimulator is on. The team will teach you how and when to change the setting. Programming the DBS system takes time. The result will be the best relief of symptoms with the fewest side effects.
Adjusting your child’s medications
As your child’s symptoms improve, the neurology team may begin to reduce their medications. The medications must not be stopped suddenly, so please carefully follow any instructions to slowly reduce medications.
Long-term follow-up
Even after the DBS stimulation settings have been optimized, your child will continue to have regular follow-up with the DBS team and neurologists.
At the age of 18, your child’s care will be transferred to an adult care centre/hospital. There will be a specialty neurology team that will continue care for the DBS programming. If there is a future need to replace the IPG battery, your child will be connected to a neurosurgeon at their new care centre who can perform the replacement.
Checking the IPG battery
The rechargeable battery lasts 15 years. The non-rechargeable battery lasts between 2 to 6 years, depending on the amount of energy used. Each time your child visits the DBS clinic, the battery will be checked. You will learn how to check it with your remote control.
There are other types of batteries that can be used for DBS as this technology evolves.
Frequently asked questions
Can my child use household electrical appliances if they have DBS?
Yes, your child can use household equipment. Using everyday electrical and electronic devices does not affect how the IPG works.
Will my child feel the electricity in their body when the IPG is working?
Some people might have a tingling feeling for a few seconds after the device is turned on, but this goes away within seconds.
Will the IPG activate metal detectors at the airport?
Yes, the IPG will set off the alarm and the security equipment may turn the neurostimulator off. You should tell security that your child has an IPG and should not go through a metal detector and show them your child’s DBS registration card. Most airport security personnel will let your child bypass the metal detector.
What if my child needs electrical shock for resuscitation?
If your child needs heart resuscitation, it should be done. The most common result is that the IPG might break and will need to be replaced.
What happens if my child needs a heart pacemaker in the future?
Your child can have both a DBS system and a heart pacemaker. Both devices can work without interfering with each other. Tell any surgeon that your child carries a DBS system.
When to call your child’s neurosurgery team
Contact your child’s neurosurgery team as soon as possible if you notice the following:
- Signs of infection
- Problems with the incision site
- Skin breakdown or erosion over the stimulator site
When to go to the emergency department after surgery
Go to your nearest emergency department if you notice the following:
- Any sudden, unexpected change in your child’s health
- Signs of infection
If your child is a patient at SickKids, please take a look at the following links:
On the day of your child’s surgery, come to the Pre-Operative Care Unit (POCU) on the 2nd floor at 6:00am. Please bring:
- Your child’s Ontario Health Card (OHIP)
- You may want to bring personal items, such as toys or blankets
- Prepare for a day-long surgery
Transition to adult care - At the age of 18, your child’s care will be transferred to Toronto Western Hospital. There will be a specialty neurology team that will continue care for the DBS programming. If there is a future need to replace the IPG battery, you will be connected to a neurosurgeon at Toronto Western Hospital who can perform the replacement.
If you have questions, please ask a member of your health-care team during your appointments or contact the clinic.
| Contact | Role | Phone/E-mail |
|---|---|---|
| Neurologists |
Dr. Alfonso Fasano Dr. Carolina Gorodetsky |
|
| Neurosurgeons | Dr. George Ibrahim |
|
| DBS Nursing Team | Sara Breitbart, Nurse Practitioner | Sara.breitbart@sickkids.ca |
| Neurosurgery Clinic | For appointment changes and inquiries | 416-813-5222 |