What is sickle cell disease (SCD)?
Sickle cell disease (SCD) is a group of inherited blood disorders that stop blood flowing normally in the body.
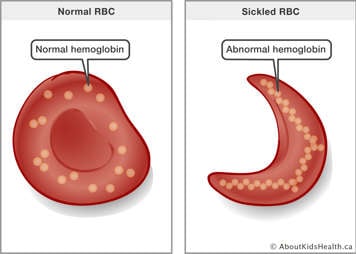
Hemoglobin is the main ingredient in red blood cells. Its job is to help the blood carry oxygen from the lungs to other parts of the body. There are different types of hemoglobin, including hemoglobin A (normal hemoglobin) and hemoglobin C and S (abnormal types of hemoglobin.
Normal red blood cells have mostly hemoglobin A, which helps keep them soft and round so they flow easily through small blood vessels. People with sickle cell disease, however, have mostly hemoglobin S (also called sickle hemoglobin). Hemoglobin S can form hard fibres inside the red blood cells, causing them to reshape into sickle (banana) shapes. When red blood cells are curved like this, they cannot move through blood vessels easily. Sometimes they even get stuck and are unable to deliver oxygen to some body tissues.
Signs and symptoms of sickle cell disease
The two main characteristics of SCD are a long-standing anemia and recurrent episodes of vaso-occlusion:
Anemia is caused by a lack of either hemoglobin or red blood cells in the body. When this happens, not enough oxygen gets delivered to the body. This can cause paleness, tiredness or fatigue, and weakness. For example, your child may become tired sooner than their peers when doing an activity. Your child may also have a hard time concentrating.
Sickle-shaped cells do not live as long as regular red blood cells. They die faster, resulting in an increased breakdown of red blood cells. The liver sometimes cannot keep up with filtering all the broken-down cells, and the bilirubin from the broken-down cells can build up in the system, making the whites of the eyes appear yellow from time to time.

- Vaso-occlusive episodes are blockages of the blood vessels anywhere in the body caused by deformed red blood cells. Sickle-shaped red blood cells cannot flow through the body as well as regular red blood cells and tend to clump together. This leads to blockages and a lack of oxygen in the affected area of the body. Symptoms depend on where the blood vessels are blocked. If the blood vessel going to a leg bone is blocked, then there will be pain in the leg. If a blood vessel going to the brain is blocked, then there will be symptoms of a stroke, such as weakness on one side of the body.

Other complications in children with sickle cell disease include acute chest syndrome, infection and enlarged spleen (splenic sequestration).
Pain episodes
The most common symptom of a vaso-occlusive episode is bone pain. Any bone can be affected, including the arms, legs, back and skull. These episodes, commonly called pain crises, are unpredictable. Some children feel unwell before the actual onset of pain and can let an adult know.
Possible triggers for pain episodes include:
- infection
- stress/fatigue
- dehydration
- exposure to cold and very hot temperatures
Some pain episodes happen without a known reason.
Preventing pain episodes
You can help prevent a pain episode by:
- Giving your child lots of fluids to drink so they are not thirsty.
- Dressing your child in a few layers of warm clothing in the winter when they are leaving home.
- Sending an extra sweatshirt and socks to school with your child in case they become wet during recess or at any other time.
- Recognizing fever as a sign of infection and having your child seen immediately by a health-care provider.
- Making sure your child avoids vigorous exercise without the ability to take breaks and drink fluids, especially during hot days.
Even with these measures, though, children may still have a pain episode.
How does someone get sickle cell disease?
SCD is always inherited (passed down in families). It is not contagious: you cannot spread it like a cold, and you cannot catch it from someone else.
How common is sickle cell disease?
SCD is the most common inherited blood disorder in the United States and Canada. It is more common in people with an African or Caribbean background, but children of Middle Eastern, Mediterranean and South Asian ancestry are also affected.
Treatment
See Sickle cell disease: What to do if your child is unwell to understand how to help your child if they are not feeling well. Find information about:
- Temperature
- Pain assessment
- Pain management
- Medications
- Physical strategies
- Psychological strategies
With SCD, the spleen function is not as good at destroying the cell coating of some bacteria. They should be receiving additional vaccinations to prevent infections caused by the pneumococcal and meningococcal bacteria. If your child is under the age of five, they should be on preventative antibiotics. The most commonly used preventative antibiotic is called
amoxicillin.
Fever in a child with SCD is considered an emergency and requires prompt treatment with antibiotics. Fever is a sign of infection.
A thermometer must be available at home for assessing the temperature of your child if they are feeling unwell. A temperature higher than 38°C under the arm and higher than 38.5°C by mouth requires that they be seen promptly at an emergency department.
Medicines such as acetaminophen and ibuprofen will reduce fever but will not treat the infection that is causing the fever. Using them can lead to a false sense of security or to the fever not being taken seriously. These medicines should only be given to your child to reduce fever after an assessment by a health-care provider.
Fluid requirements for children with sickle cell disease
Children with SCD excrete higher volumes of urine compared with their peers because their kidneys cannot concentrate urine.
Correspondingly, when a child produces more urine than usual, they must also increase their fluid intake. This is particularly important in SCD, as dehydration can trigger pain episodes. When a child with SCD is dehydrated, blood cells also become dehydrated and change shape, causing blood vessel blockage and acute pain. Make sure your child has easy access to water at all times.
Other treatments and medications for sickle cell disease
Your child may receive sickle cell treatments in hospital to prevent complications and medications to target sickle cells, infections and pain. To learn more about these treatments, please see Sickle cell disease: Types of treatments and medications.
Special situations where parents should call 9-1-1
If any of the following occurs, seek immediate medical attention or call 9-1-1 right away:
- difficulty breathing
- loss of consciousness
- severe headache
- difficulty speaking or slurring of speech
- weakness of limbs
- seizure activity
- fever greater than 39°C
- unexplained lethargy/sleepiness
- persistent vomiting
- recognition of an enlarged spleen