What is hemolytic uremic syndrome?
Hemolytic uremic syndrome (HUS) is a disease that affects the kidneys and other organs.
"Hemolytic" means "blood breakdown." "Uremic" means "urea in the blood" (urea is a waste product). So HUS is a condition where the blood breaks down and waste products build up in the blood. HUS is very serious, but with proper care most children recover completely.
This page explains what HUS is, how it affects your child, and what to expect during treatment.
How hemolytic uremic syndrome affects the body
HUS most often affects the kidneys, the blood and the brain.
The kidneys
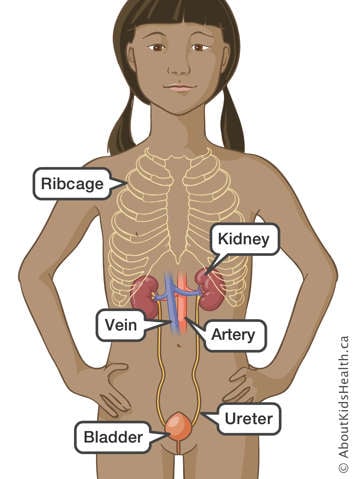
Most people are born with two kidneys. The kidneys take excess water and chemical waste products out of the blood and turn them into urine (pee). The urine then flows out of the body.
When a child has HUS, the kidneys cannot clean the blood properly or make the normal amount of urine. Extra fluid and chemical wastes build up in the body. This can cause several problems:
- If fluid builds up in the blood vessels, your child's blood pressure will rise.
- If fluid builds up in the soft tissues, your child will have puffiness and swelling.
- If fluid builds up in the lungs, your child will have trouble breathing.
- If the waste product potassium builds up in the blood, it may cause an irregular heartbeat or even stop the heart from beating.
- If the waste product urea builds up in the blood, it may make your child sleepy or irritable (cranky). It may also make your child's breath smell bad.
If HUS progresses, the kidneys can stop working, and you may see changes in how your child behaves. For example, they may urinate less and be less hungry.
The blood
Our blood contains three different types of cells:
- Red blood cells carry oxygen around the body to all our tissues and organs.
- White blood cells help fight infection.
- Platelets are "sticky cells" that help the blood to clot.
As the blood flows through inflamed blood vessels, the red blood cells and platelets may be broken down.
- A low platelet count can be associated with bruising and easy bleeding. Nosebleeds or bleeding from the gums are common signs of a low platelet count.
- A low red blood cell count is called anemia. Children with anemia may look pale and feel tired.
The brain
HUS may increase blood pressure and affect the blood vessels in the brain. This can make your child cranky, tired and more demanding. In severe cases, your child can have seizures, where they cannot control their movement and may lose consciousness. Seizures can be controlled with medicine. They usually disappear when a child recovers from HUS.
Symptoms of hemolytic uremic syndrome
Early symptoms
If your child has an E. coli O157 infection, they may throw up, have diarrhea, feel weak or feel sick to their stomach. HUS is not usually diagnosed at this early stage. This is because these symptoms are seen with many causes of infectious diarrhea.
Later symptoms
These are some signs of HUS that appear after several days:
- blood in the urine
- blood in the stool (bowel movement or poo)
- bruises that are not caused by injuries
- less urine
- puffiness around the eyes and ankles
- paleness
- higher blood pressure
- sleepiness
- irritability
- headaches
- seizures
The doctor will take blood samples to find out if your child has HUS.
Cause of hemolytic uremic syndrome
HUS most commonly follows an infection of the intestines
HUS is usually caused by a bacteria called E. coli O157:H7. Healthy people have several types of E. coli living in their intestines. E. coli O157:H7 is a different strain that can be very harmful. It can come from contaminated food, drink, or another source, including other people who are sick with the infection. Undercooked hamburger is one common source, so HUS is also called Hamburger Disease.
Most people who swallow this bacteria will get gastroenteritis. Gastroenteritis causes diarrhea, cramps and vomiting (throwing up). Anybody can get E. coli O157:H7 gastroenteritis, but it is most serious in children and elderly people. About one in 10 children who have E. coli O157:H7 gastroenteritis will go on to develop HUS.
Some forms of HUS are not associated with diarrhea
Another form of HUS is known as atypical HUS or D- HUS (diarrhea-negative HUS). This is a more serious illness that is sometimes caused by inherited disorders. It may have a different course than diarrhea-associated HUS.
How hemolytic uremic syndrome is treated in the hospital
Your child might need to be isolated for a while
HUS is started by an infection. It is possible for a child with HUS to give the E. coli O157 bacteria to someone else, who would then be at risk for developing HUS as well. For this reason, all children with HUS are kept by themselves (isolated) until several stool samples are negative for the bacteria.
Children with HUS may be in a single room or with other children who have HUS. They can only have a limited number of visitors at any one time. Visitors will need to check in at the nursing station. Your child's nurse will explain to you the rules of isolation.
Here are things that you can do to make sure HUS is not passed on to others:
- Wash your hands very well before and after you touch your child.
- Do not eat or drink anything in your child's room.
- Watch for symptoms of HUS in other family members.
- Tell the nurse or doctor right away if you or others get HUS symptoms.
- Visitors who want to see your child must check in at the nursing station.
Hospital staff will watch your child's blood pressure, blood work, urine and stools
Your child's blood pressure will be checked many times a day. Children with HUS often have high blood pressure and need medicine to lower it. High blood pressure must be treated, because it can harm the kidneys and cause other problems.
Blood tests will be done several times a day. These tests show how the disease is progressing and help doctors decide on medicines and other treatments for your child.
Children with HUS often have low hemoglobin because their red blood cells are being broken down. Hemoglobin is the substance that carries oxygen around your child's body. If your child has low hemoglobin, they may need a blood transfusion. This means your child will be given blood to keep their hemoglobin from falling too low, which can cause a strain on the heart. The blood comes from a blood donor.
Samples of urine and stools will be taken to check for blood, bacteria or viruses.
The nurse will record how much fluid your child takes in
Your child may get fluids through an intravenous (IV) tube. This is a small tube put in a vein in the arm. It is used to give liquids or medicine to your child.
The nurse will write down how much fluid your child drinks and how much they get as IV fluids. The nurse will also write down how much fluid your child gets rid of in urine, diarrhea or vomit. Always tell your child's nurse:
- when your child eats or drinks
- when your child goes to the bathroom
- when your child throws up
Because your child's kidneys are not working well, the doctor might limit how much fluid your child can have. You will be told how much they are allowed to drink. You must be careful to record exactly how much they drink. Do not give them more fluid than they are allowed.
For more information, please read Restricting fluids.
Your child may need a special diet
Children with HUS often need a special diet. The most common diet for HUS has no added salt, low potassium, low phosphorus and low protein.
At first, your child will not want to eat very much. Your child may need to be fed by IV until they can eat enough by mouth, because the body needs good nutrition to get better.
When your child wants to eat by mouth, a dietitian will help plan your child's menu. They will tell you which foods your child can and cannot eat. Make sure your child follows the special diet.
Your child may need dialysis
Dialysis is a common treatment for HUS. A dialysis machine removes water and chemical wastes from the blood and returns clean blood to the body. Dialysis takes over most of the work of the kidneys while the kidneys are getting better. Usually dialysis is started soon after diagnosis. It can go on for two to three weeks or even longer.
There are two main types of dialysis: hemodialysis and peritoneal dialysis. If your child needs dialysis, you will be given more information at that time. Your child's doctor will tell you which type of dialysis is right for them.
For more information, please read Dialysis.
Outcome: going home
Most children recover completely from HUS. How long your child stays in hospital will depend on the symptoms, how they respond to treatment and how quickly their kidney function improves. You will still need to visit your hospital's nephrology clinic regularly so that your child's progress can be checked.
If you have questions, please talk about them with your child's nurse or doctor.