The retina is the light-sensitive lining at the back of the eyeball. Over time, having diabetes damages blood vessels (arterioles and veins) in the retina. This is called diabetic retinopathy.
Eye damage (retinopathy)
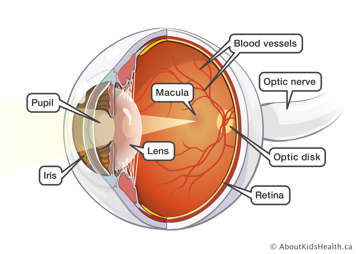
Diabetic retinopathy can lead to bleeding or leaking. It tends to start quietly and slowly. People usually keep their ability to see until the condition worsens. The only way to see changes is with a careful eye exam by an experienced ophthalmologist or optometrist. Ophthalmologists and optometrists are doctors who specialize in eye care. The eye exam should involve eye drops that widen the pupil so that the retina can be fully seen.
Damage to the retina can be either proliferative or non-proliferative.
Proliferative means that new, abnormal blood vessels have started to form. These blood vessels tend to be weaker and they sometimes bleed or leak.
In non-proliferative disease, the same problems happen with the blood vessels that are already there.

Early changes in diabetic retinopathy
The earliest changes are often non-proliferative retinopathy. This consists of little swellings of the blood vessels, called microaneurysms. They may start to leak or bleed.
Later changes in diabetic retinopathy
Retinopathy may progress to proliferative retinopathy. Unfortunately, some people may start with proliferative retinopathy. In this later stage, the eye begins to make new blood vessels in an attempt to provide better blood flow. These new vessels are fragile. They may cause bleeding and scarring in the fluid chambers of the eye in front of the retina.
The scarring due to bleeding can cause the retina to separate or pull away from the eye. Proliferative retinopathy and its effects are a major cause of partial or complete loss of sight.
There are often no signs early on. Later, signs of diabetic retinopathy include:
- 'floaters' or spots in your vision
- decreased sight.
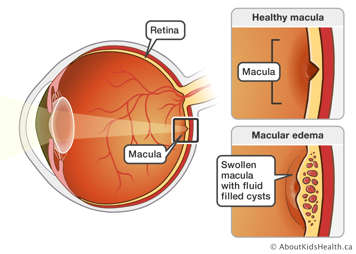
Diabetic macular edema
Diabetic macular edema occurs when there is thickening and swelling of the retina at the macula. The macula is the part of the retina responsible for sharp vision.
Diabetic macular edema tends to happen with more severe retinopathy, but it can also happen at early stages.
Diabetic macular edema
What can be done for diabetic retinopathy?
A lot can be done to repair vision and reduce the risk of blindness in people with diabetes. Photocoagulation is a laser therapy technique that prevents blindness. It destroys abnormal blood vessels, repairs leaking ones and stops new vessels from forming. This can greatly reduce the risk of blindness. There are also medications that can be delivered directly to the eye, which can help in certain situations. Occasionally, surgery may be needed if the retina has bled too much or has become detached.
Cataracts
A cataract is a thickening in the lens of the eye. Cataracts cause blurry vision. Young people with type 1 diabetes very rarely have cataracts, but they can develop at any time.
Surgery can remove cataracts. Glasses or contact lenses can correct remaining sight problems.
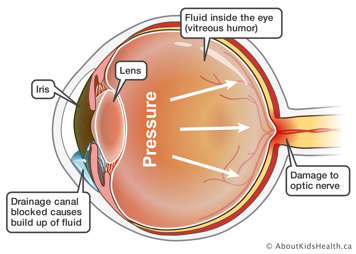
Glaucoma
Glaucoma often occurs when there is increased pressure in the eye. This damages the optic nerve. The optic nerve allows us to see by bringing signals from the retina to the brain.
Glasses
Children with diabetes are as likely as their friends without diabetes to need glasses.
Sometimes rapid changes in blood glucose (sugar) levels can cause changes to the lens of the eye. The lens can swell if the sugar level rises too much; it can shrink if the sugar level drops quickly. This can cause temporary blurry vision. Balancing the blood sugar level will correct this situation.
Any child who complains of problems seeing the board in the classroom, or who has to sit close to the television, should have an eye exam to see if they need glasses.