What is a corneal transplant?
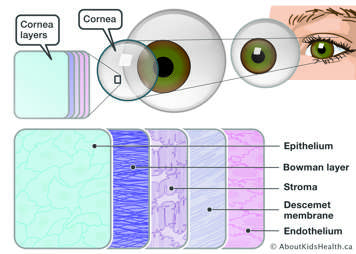
A corneal transplant is an operation to replace a cloudy or scarred cornea or a poorly functioning part of the cornea, with a clear, healthy cornea. The type of transplant depends on the eye disease or injury and the preference of the corneal surgeon. Corneal transplantation may be full thickness, where all the layers of the cornea are replaced. Another cornea transplant option is a partial thickness corneal transplant, such as Descemet membrane endothelial keratoplasty (DMEK), in which the corneal surgeon replaces only the diseased or poorly functioning innermost layer of the cornea.
The healthy corneal tissue comes from a donor. A donor is a person who gives their eyes, after dying, to help others such as your child.
Your child needs a corneal transplant if your child's cornea is cloudy
If your child's cornea is cloudy, it can affect how well your child sees. A cloudy cornea will make your child's eyesight blurry. The amount of blurriness depends on how cloudy your child's cornea is.
Your child may need a corneal transplant if the cornea is cloudy because of any of these problems:
- an injury to the eye
- a very bad eye infection
- swelling of the cornea
- a cloudy cornea that your child was born with
- a thin cornea
- a cornea that bulges outward
- a previous corneal transplant that is no longer working
Corneal transplant procedures
- Penetrating keratoplasty (PKP) is a full-thickness transplant procedure, in which a full-thickness portion of the child’s cornea is removed and replaced with the full-thickness donor corneal graft.
- Descemet stripping automated endothelial keratoplasty (DSAEK) uses donor tissue to replace the inner layer of the cornea.
- Descemet membrane endothelial keratoplasty (DMEK) replaces the inner layer of the cornea and uses a much thinner layer of donor tissue.
- Deep anterior lamellar transplant (DALK) replaces the front and middle layers of the damaged cornea extending deeper into the stroma (main bulk of cornea).
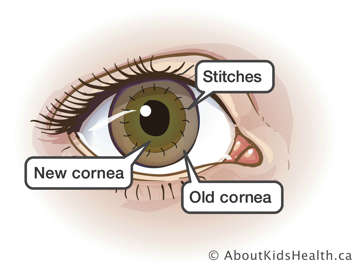
In all of these procedures, a small button-sized healthy corneal tissue from the donor is attached (grafted) to replace the removed portion.
About 90% of all corneal transplant procedures are successful in restoring vision and corneal clarity.
If the procedure is unsuccessful, the surgeon may perform a second corneal transplant which has a success rate of 70%. What you can expect after your cornea transplant depends on the reason for your child’s surgery and your child’s health.
Problems that may happen after a corneal transplant are:
- infection
- rejection of the donor cornea
- problems with the stitches used to secure the donor cornea
- glaucoma (increased pressure in the eye)
- increased risk of clouding of the eye's lens (cataract)
- bleeding
- detached retina (tissue lining the inside of the eyes pulls away from the eye)
- astigmatism (irregular corneal curviture; may need to wear glasses or contact lenses)
Before cornea transplant surgery
Before cornea transplant surgery, your child will have a thorough eye exam. During the eye exam, the doctor will:
- look for conditions that may cause complications after surgery
- check your child’s eye and check what size donor cornea will be needed
- review any medication and ensure that your child continues or stops taking certain medications
Treatment for other eye problems and unrelated eye problems may be started. Conditions such as infection or inflammation may reduce the chances of a successful cornea transplant. The eye doctor will treat these problems before the surgery.
Giving consent before the procedure
Before the transplant procedure, the eye doctor will go over how and why the procedure is done, as well as the potential benefits and risks. The doctor will also discuss what will be done to reduce these risks. It is important that you understand all of these potential risks and benefits and that all of your questions are answered. If you agree to the procedure, you can give consent for treatment by signing the consent form. A parent or legal guardian must sign the consent form for young children. The procedure will not be done unless your consent is given.
Preparing for the procedure
Your child will be asleep during the surgery. Please see the articles, Sedation and General anaesthesia for information on what to expect and how to prepare before sedation or general anaesthetic.
The new cornea
The new cornea will not change the colour of your child's eyes, because the cornea is clear. The corneal transplant will make the natural colour of your child's eye clearer.
The ethnicity, sex and eye colour of the donor do not affect how your child sees after the corneal transplant.
For a corneal transplant, the donor tissue or blood type does not have to match that of your child. The human cornea is avascular, meaning that it does not have blood vessels.
Your child has little or no chance of getting a disease from a corneal transplant. All tissues from donors are tested for contagious diseases, such as AIDS and hepatitis (a disease of the liver).
A corneal transplant should be done when vision is severely affected
Early treatment helps your child's eye grow and helps eyesight develop properly. The doctor will talk to you about the exact time that your child should have a corneal transplant.
Your child will probably go home on the same day as the operation
Your child is asleep during the surgery and does not feel any pain. Your child will go home on the same day they have the operation, unless they are very young.
Your child will wake up with a patch and shield on the eye. This should stay in place for the first day. The doctor will take the patch off and examine one eye on day one. Check the eye and start eye drops as prescribed.
Possible complications of corneal transplant
Corneal rejection can happen when the body’s immune system sees transplanted tissue as something that should not be there and tries to get rid of it. Rejection is a problem for up to three out of 10 people who have a corneal transplant.
Signs of corneal rejection
Tell the eye doctor right away if your child has any of the following signs.
- loss of vision
- pain
- redness
- change in appearance of the transplant
- sensitivity to light
The doctor may be able to stop the rejection with medicine.
Caring for the eye after the corneal transplant
After the corneal transplant, the doctor will put a patch and a shield over your child's eye. These protect your child’s eye as it heals after the surgery.
The doctor will take off the patch and shield the next day and look at your child's eye.
Your child will take eye drops and medicine after the corneal transplant
The doctor will let you know what medicine you can use for pain, if needed. Most children do not have much pain after a corneal transplant.
The doctor will order eye drops or eye ointment for your child. Eye ointment is a thick gel. Your child may need to use these eye drops or eye ointments for several months.
Your child will need these medications to:
- help the cornea heal
- reduce swelling, redness and pain
- prevent or control infection
How to give your child the medicine
- Do not force your child's eyelid open when you give your child any of these medicines. Forcing the eyelid open puts pressure on the new cornea. You will be told how to do it, or a nurse will show you.
- Learn the names and doses of all your child’s medicines.
- Give all medicines exactly as directed.
- Confirm changes to medicines at every clinic visit.
- If your child misses a dose, inform your doctor immediately.
- Keep medicines in a dry place, away from heat and light.
- Report any side effects to your doctor.
Protect the eye from injury
Your child's eyesight will improve slowly. How well your child sees depends on how much the eye was affected before the corneal transplant.
Extra precautions to avoid harming the eye
- Your child should not touch, rub or put any pressure on the eye.
- Your child should lie on their back, facing the ceiling for 48 hours after the transplant (only for DMEK or DSAEK).
- Let your child take it easy after the transplant and slowly work their way up to normal activities. They should not do exercise or physical activities for at least 30 days or as recommended by their doctor.
- Your child can take a shower or bath and shampoo their hair after a few days.
- Your child can watch television or use an electronic device. This will not hurt the eye.
- In cases where a gas or air bubble is injected in the eye, it will not be possible to fly until the bubble has been reabsorbed.
Older children or teens may return to school, work or their normal routine in about one to two weeks after surgery. Your child’s vision will still be blurry.
Your child will see the doctor after the corneal transplant
The doctor will see your child frequently after the corneal transplant: the day after the corneal transplant, then weekly or as often as your child needs to.
Your child will keep seeing the doctor, even after the cornea is healed. The doctor will check your child's eyesight for any changes and any sign of problems.
The doctor will take your child's stitches out at least a month after the operation
The stitches that hold the new cornea in place are very small and are very difficult to see.
When your child's stitches can come out depends on how well the cornea is healing. Sometimes the doctor will take them out as early as one month after the operation. The stitches may be removed all at once, or they may be removed slowly over months.
The doctor will decide later if your child needs glasses or contact lenses
Your child's vision may initially be worse than before surgery. However, as the eye adjusts to the new cornea, your child’s vision will improve. Your child's eyesight will continue to change for months or years after this operation.
When the outer layer of your cornea has healed and the stitches come out, the eye doctor will work to help the vision by correcting refractive errors. Refractive errors, such as nearsightedness and farsightedness, can be corrected with glasses, contact lenses or, in some cases, laser eye surgery.
Your child will be tested for other eye diseases
Your child will have many follow-up examinations. During these examinations, your child will be tested for:
- Unevenness in the cornea (astigmatism). The stitches that hold the donor cornea in place on the eye may cause dips and bumps in the cornea, making the vision blurry. The doctor may correct some of this by releasing some stitches.
- During the examination, your child will be tested for glaucoma and amblyopia. Glaucoma is caused by too much fluid collecting inside the eye. It can damage the optic nerve, which carries information about what we see from the eye to the brain. Amblyopia is a condition in which one eye loses the ability to see clearly. Amblyopia is caused by any condition that causes one eye to be favoured. The favoured eye usually has normal vision.
Watch for signs of complications at home
Watch for these warning signs that your child's body is rejecting or trying to get rid of the new cornea or that the eye is infected. Call the doctor right away if you see any of these warning signs:
- Your child has pain in the eye that will not go away with pain medicine.
- Your child is bothered by light more than they usually are.
- Your child's eye is red, especially around the cornea.
- A sticky liquid is draining from the eye.
- Your child's eye has blood in it. Note that a small amount of blood on the eye patch or in the tears is normal in the early days after surgery.
- Your child's eye is swollen.
- Your child’s vision is cloudy or hazy.
- Your child tells you their eyesight has become worse.
If your child's new cornea does not work and cannot be saved, your child might need another corneal transplant.
For more information or help
If you have an emergency or if you have any concerns about your child's transplant, call your doctor or the eye doctor on call at 416-813-7500 or go to the emergency department at The Hospital for Sick Children.
Resources
For more information about the eyes, please see Eye anatomy and function.