What is coarctation of the aorta?
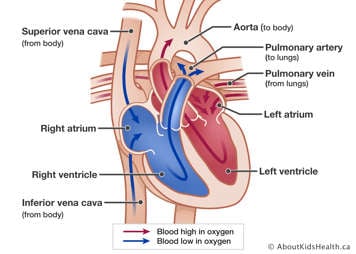
The aorta is the main artery that carries oxygenated blood from the left ventricle of the heart to the body, supplying the body’s organs with blood.
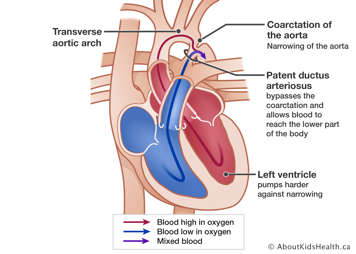
Coarctation of the aorta means the aorta has a narrowing. This condition is present at birth (congenital). It most commonly occurs in a small area of the aorta called the isthmus or 'juxtaductal' region. In some cases, longer sections of the aorta can also be narrowed. This is called transverse arch hypoplasia. The narrowing of the aorta causes a blockage for blood leaving the left ventricle, which means the heart has to work harder to pump the blood through the aorta. In a baby, if the narrowing is very severe, it can cause the left ventricle to fail. A ductus arteriosus allows the blood to bypass the narrowed section of the aorta to reach the body. The ductus arteriosus is patent (open) at birth and typically shrinks and closes within the first few days of life.
Sometimes, people with coarctation have other heart defects, such as a ventricular septal defect, or a bicuspid aortic valve.
How is coarctation diagnosed?
Coarctation of the aorta is present from birth, but the age at which it is diagnosed usually depends on how severe the narrowing of the aorta is. Babies may not have symptoms at birth and start developing symptoms when the ductus arteriosus closes. If it is severe, babies can become very sick within the first month of life and need admission to hospital. If the narrowing is less severe, it may not be detected for many months or even years. In an older infant, adolescent or sometimes adult, a heart murmur or high blood pressure can indicate an undiagnosed coarctation.
The diagnosis is most often confirmed by using an echocardiogram. A computed tomography (CT) or magnetic resonance imaging (MRI) scan, and occasionally a heart catheterization may also be used to confirm diagnosis. Coarctation in a fetus may be identified during pregnancy by performing an echocardiogram of the fetus’ heart, however this is a difficult heart condition to detect due to the unique fetal heart circulation.
How is coarctation treated?
Treatment depends on how severe the narrowing of the aorta is. In a baby with a severe coarctation who becomes sick within the first few months of life, an operation is required to remove the narrowed section of the aorta. The two healthy parts of the aorta are then connected. This operation is usually performed through the ribs on the left side of the chest, with an incision called a left thoracotomy. If the narrowing of the aorta extends into the transverse arch or if the baby has other heart defects such as a ventricular septal defect, the operation is usually performed through the middle of the chest (sternum), with an incision called a midline sternotomy.
An alternative option to surgery is a heart catheterization procedure. During this procedure a thin, flexible tube called a catheter is inserted into a blood vessel in the groin that leads to the heart. A balloon is inflated inside the aorta to widen the narrowed area. Catheterizations are typically only for patients who are older than 3 months or for whom the coarctation is less severe. Sometimes, in older children a stent (small metal tube) is placed in the aorta to help keep the narrowed section open. As the child gets older, this stent may need to be dilated during a catheterization procedure.
Complications of coarctation of the aorta
Aortic coarctation, like all congenital heart disease, is a lifelong condition and while treatment is usually successful, some complications can develop. Therefore, it is important to keep seeing a cardiologist regularly as many of these complications can be detected before symptoms develop.
Re-coarctation
Sometimes, the narrowed area in the aorta comes back. This is called re-coarctation. If this happens, another operation or a heart catheterization to open the narrowing may be needed. This happens in about 5% of patients. Re-coarctation can be detected by measuring the blood pressure in the arms and legs, or by echocardiogram, CT or MRI scan. The risk of re-coarctation is highest within the first year after surgery.
Hypertension
Those with a coarctation have a higher risk of developing high blood pressure (hypertension), even if the narrowed section of the aorta was repaired successfully. The blood pressure can be normal at rest but can become very high during exercise. High blood pressure can be detected by a machine which measures blood pressure for 24 hours. Medication may be needed to control blood pressure.
Aneurysms
Rarely, in some individuals with coarctation, aneurysms can develop in the aorta or the brain. Aneurysms are swollen blood vessels which sometimes become too big and possibly burst. This is a very serious complication . Aneurysms can be detected by echocardiogram, CT or MRI scans of the aorta or the brain. Routine visits to the cardiologist are important as they allow for these problems to be diagnosed and treated early. Aneurysms are more common in those who had an aortic coarctation repair as adults or have uncontrolled high blood pressure.
Endocarditis
Children with coarctation can be at risk of infection of the heart or aorta (endocarditis). If a stent was implanted or a graft was used to repair the coarctation, there is a risk of endocarditis for 6 months after the procedure. Antibiotics will be needed before certain medical or dental procedures.
What is the long-term outlook for children with coarctation of the aorta?
Can children with aortic coarctation exercise normally?
Regular exercise is important to keep both the heart and the mind healthy. In the past, children with congenital heart disease were often told not to exercise, or to not push too hard during exercise as the heart was weak. However, it is now known that for most children with congenital heart disease, regular exercise is beneficial to their overall health. Most children who had a successful coarctation repair can exercise normally and participate in all competitive sports, with some exceptions.
- Children who have had a recent surgery should wait 3 months before returning to sports. Those who have had a catheterization should wait 1 month before returning to sports. Those with aneurysms in their aorta might not be able to participate in contact sports.
- It is recommended to avoid high-intensity weightlifting, even if the coarctation repair was successful. Participation in lower volume weightlifting is allowed. As a general rule, it is safe to choose a weight that can be performed in 10-12 repetitions over 3-4 sets. This type of exercise is called 'static' training.
Speak with your child’s cardiologist or transition nurse to discuss safe participation in sports and activities.
If I have children will they have congenital heart disease too?
The risk for any person having a baby with congenital heart disease is about 1%. For babies born to a parent who has congenital heart disease, such as a coarctation, the chance that the baby will have any type of congenital heart disease is about 3%. This risk is for both men and women. That still means there is a 97% chance that the baby will not have congenital heart disease.
Women with congenital heart disease can talk with a genetic counselor or genetic specialist before becoming pregnant. An ultrasound scan of the fetus' heart can be performed during the pregnancy to look for congenital heart disease if either parent has congenital heart disease.
