What is a pacemaker?
A pacemaker is a small device that uses electrical impulses to control the speed and rhythm of your child's heartbeat. A pacemaker is surgically placed (implanted) in the body. It has two parts:
- The pacemaker itself is a metal box with a battery. It delivers electrical impulses to the leads.
- The leads are wires connected to the pacemaker. They carry the electrical impulses to the heart muscle.
Preparing for an operation to put in a pacemaker
Speak to your child about what is going to happen
What, when and how you tell your child about the operation for a pacemaker will depend on how grown up and mature your child is. Talk to your child in a way that they can understand. You can use the information on this page as a start.
A few days before the operation, let your child know that they will be going to the hospital for an operation. It is important to be honest. Your child will feel less anxious and scared when they know what to expect. Children also take their behavioural cues from the adults around them. If you speak to your child in a calm manner without anxiety about the upcoming operation, your child will feel less anxious and scared.
Let your child know that they may have pain and needles before and after the operation. Comfort your child and let them know that you will be with them as much as you can. Your child should also understand that the operation is needed and that the doctors and nurses are there to help.
Your child will need to stay in the hospital for a few days. You can stay with your child during this time.
Clinic visit before the operation
Your child will need to visit the cardiac pre-operative clinic a few days before the operation. During this visit, the nurses will let you and your child know more about the operation. The doctor will also discuss the details of the operation with you, including how the surgery will be done, where the incision (surgical cut) will be made, and the risks of the operation.
Your child may also need one or more of the following tests:
- an electrocardiogram, also called an ECG, which measures and records the electrical activity in the heart
- blood tests
- a chest X-ray, which takes a picture of your child's heart
- an echocardiogram, which is a type of ultrasound that can take moving pictures of the heart's muscles and valves at work
Eating and drinking before the operation
Your child must stop eating and drinking several hours before the operation. The table below tells you when your child must stop eating and drinking. The nurse will discuss this with you during your clinic visit to the hospital before the operation.
What your child can eat and drink before the operation
| Time before procedure | What you need to know |
|---|---|
| Midnight before the procedure | No more solid food. This also means no gum or candy. Your child can still drink liquids such as milk, orange juice and clear liquids. Clear liquids are anything you can see through, such as apple juice, ginger ale or water. Your child can also eat Jell-O or popsicles. |
| 6 hours | No more milk, formula or liquids you cannot see through, such as milk, orange juice and cola. |
| 4 hours | Stop breastfeeding your baby. |
| 2 hours | No more clear liquids. This means no more apple juice, water, ginger ale, Jell-O or popsicles. |
A team of professionals will perform the operation at the hospital
Your child's surgery will be performed at the hospital, in a special laboratory or operating room. Doctors, nurses and an anaesthetist will all help during the operation. An anaesthetist is a doctor who is specially trained to give anaesthetics, the medicines that keep your child asleep and feeling no pain during the operation.
The morning of the operation
Your child will be admitted to the Cardiology Inpatient Unit. To get ready for the operation, your child will be given an intravenous (IV) tube. An IV is a small tube put in the vein of an arm or leg so that the doctors can easily give your child medicines.
During the operation
Your child will be given a general anaesthetic to put your child to sleep during the operation.
Sticky pads may be placed on your child's chest at the beginning of the operation. If necessary, these pads can be used to maintain your child's steady heart beat during the operation.
During the operation, the doctor will put in a pacemaker or replace your child's current pacemaker. There are two types of pacemakers your child may receive: a transvenous pacemaker, or an epicardial pacemaker.
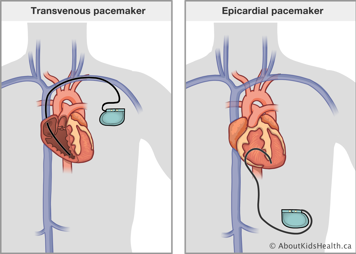
Operation to put in a transvenous pacemaker
- A special catheter may be passed through a vein in the groin if your child needs temporary pacing during the procedure. If used, this catheter will be removed at the end of the operation.
- An incision is made in the chest. The doctor makes a pocket between the layers of muscle and inserts the pacemaker into this pocket.
- The pacemaker lead is then passed through a vein near the shoulder to the correct location inside the heart. The doctor uses special X-ray pictures called fluoroscopy to make sure the lead is put in the right place in the heart muscle.
- The doctor then connects the pacemaker to the lead and the chest incision is closed with stitches. Over time, these stitches will dissolve on their own. The incision site is covered with a bandage.
Operation to put in an epicardial pacemaker
- A small incision is made in your child's chest to put the lead(s) on the heart.
- One end of the lead is stitched on the outside surface of the heart muscle and the other end connects to the pacemaker.
- The surgeon makes a pocket between the layers of the chest wall or abdomen muscles and inserts the pacemaker into the pocket.
- The incision is then closed with stitches. Over time, these stitches will dissolve on their own. The incision site is covered with a bandage.
How much time the operation will take
Your child's surgeon will let you know how long the operation should take. The length of time will depend on what type of pacemaker is used and if there are any complications during the operation.
After the operation
After the operation, your child will be moved to a recovery room to wake up from the anaesthetic. It is likely that your child will remain in the recovery room for a couple of hours. Then they will go back to the cardiology inpatient unit. You will be able to visit your child in the recovery area once they are ready.
The doctor will come and talk to you about your child's operation.
Because of the general anaesthetic used during the operation, your child may be very sleepy for several hours. Your child may need to stay in bed for about four hours after the operation. During this time, the nurse will check your child's blood pressure, breathing and incision(s) regularly.
After your child is awake, they will be allowed to drink liquids and slowly begin eating and drinking normally again.
Your child may also have another electrocardiogram and chest X-ray.
Your child will also get antibiotics through the IV tube for about two days following the operation. These medicines fight infection.
Managing your child's pain
Your child may be sore around the incision site(s) and will receive pain-relieving medicine.
Your child may also have an upset stomach for a short time after the operation. This is likely due to the anaesthetic. If your child has an upset stomach, your child's nurse will give your child medicine to help.
Monitoring your child after the operation
The incision site(s)
The doctors and nurses will monitor your child's incision site(s) for bleeding and signs of infection. These signs include fever, redness, swelling and drainage around the incision.
Checking that the pacemaker is working properly
Your child's pacemaker will be checked with a small machine called a Holter monitor. The monitor checks your child's heartbeat. Your child will wear the Holter monitor for 12 to 24 hours following the operation.
After the doctors have the results from the Holter monitor, the pacemaker technologist will test your child's pacemaker with a small computer. The test does not hurt.
Going home
After all the tests on the pacemaker are done and your child has finished the antibiotics, your child should be ready to go home.
Before you leave, members of your child's health-care team, such as the doctor, pacemaker technologist and nurses, will teach you:
- how to care for your child with a pacemaker
- signs and symptoms to watch for
- how to tell if there is something wrong with the pacemaker
- when to seek medical attention
Follow-up visits
Your child will need regular follow-up appointments to the pacemaker clinic to make sure the pacemaker is working well. Before you leave the hospital, you will be given an appointment for your first follow-up visit.
Write the date and time of the appointment here:
Generally, the first follow-up appointment at the pacemaker clinic is between one and two months after the operation. Eventually, your child's follow-up appointments will become less frequent, such as every six months.