What is a continuous peripheral nerve block?
A continuous peripheral nerve block (CPNB) is a way of giving pain medication to your child during and after surgery. This medication is delivered directly to an area that numbs a specific part of the body and blocks pain signals so your child feels less pain.
An elastomeric device is sometimes used to deliver CPNBs. These portable devices contain a balloon filled with local anesthetic, which is a numbing medication. As the balloon deflates, a steady flow of local anesthetic is delivered around the nerves that give sensation (feeling) to the site of surgery.
With a CPNB, your child may:
- feel little to no pain around their surgical site
- be able to leave the hospital sooner, recover faster and get back to their normal activities
- be less likely to need stronger pain medications, such as opioids. This will also mean there will be fewer side effects from opioids (e.g., itchiness, drowsiness, nausea, vomiting and constipation)
Caring for your child with an elastomeric device at home
Pain management
Your child should experience little to no pain around their surgical site. Your health-care team will provide instructions about what types of pain medications can be given to manage mild pain and discomfort, and what can be given to treat stronger pain. Before going home with an elastomeric device, speak to your health-care team about a pain management plan for while the nerve block is being delivered to the site and for after the nerve block catheter is removed.
Caring for the numbed body part
The medication delivered by the elastomeric device will cause the area around your child's surgical site to have less sensation (feeling) than normal. Do not place heat or ice on the numbed body part. Help your child reposition the numbed body part every few hours to prevent skin damage.
Activity
Follow the surgical team's guidance for how much physical activity your child should be doing.
Because your child may have a numb feeling near their surgical site, it is recommended that your child is helped with movement, changing positions, bathing, and dressing. Sponge bathing is recommended to prevent the dressing and device from getting wet.
Taking care of the elastomeric device at home
The catheter insertion site and dressing
- The skin around the catheter insertion site should look clean and healthy
. - A small amount of clear fluid around the site is OK.
- The dressing should cover the entire catheter insertion site. Keep the dressing dry.
The tubing and flow meter
- Check for kinks along the entire length of the tubing. Untangle the tubing if required.
- The flow rate meter should remain at the prescribed rate.
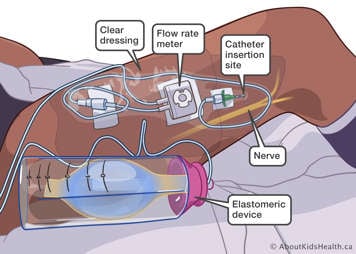
The elastomeric pump
Ensure the balloon inside the device is getting smaller. This means the medication is being delivered to the site.

- The device should be kept at about the same level as the catheter insertion site. Talk to your health-care team before going home from the hospital about some strategies for keeping the device at the correct height.
- The device should be kept at room temperature. Do not cover the device or tubing with ice packs or heating pads.
- Keep the device dry.
Removing the catheter
The elastomeric device is to be removed when the balloon is empty, usually 2 to 3 days after surgery. In some cases, you may be instructed to remove the catheter at an earlier time. The removal of the catheter is not painful but there can be some discomfort with the removal of the dressing.
- Wash your hands well with soap and water.
- Lift a corner of the dressing and stretch it along (parallel to) the skin. As it stretches, it will begin to lift off. Remove the entire dressing and any other tape used to hold the catheter in place. You may wet the edges of the dressing/tape with some warm water if this helps with removal.
- Hold the catheter as close as possible to the skin and gently pull it out. The catheter should slide out easily. If it does not, reposition your child's limb and try again. If you are still having trouble removing the catheter, call the Acute Pain Service using the contact information at the end of this article.
- Look for a blue or black marking at the tip of the catheter. Call the Acute Pain Service if there is no marking.
- Use gauze to put pressure on the catheter insertion site for one minute. Cover the site with a bandage. The bandage can be removed after 4 hours.
- Throw away the device and catheter in your household garbage.
- Wash your hands well with soap and water.
What can my child expect when the catheter is out?
After you remove the catheter, your child will slowly notice sensation (feeling) coming back to the numb area. It is normal for your child to continue to feel numbness for up to one day after you remove the catheter. If your child still feels numb 48 hours after the catheter removal, then on the next business day contact the Acute Pain Service.
Keep giving your child pain medication as directed by your surgeon and the Acute Pain Service. Return any unused prescription medications to your pharmacy.
Complications and troubleshooting
| What to assess | Details | What to do |
|---|---|---|
| Skin around the catheter insertion site | Signs of infection include:
|
Notify the Acute Pain Service if there are signs of infection. |
| Local anesthetic toxicity | Although VERY RARE, local anesthetic toxicity can happen. This is when medication from the catheter gets into the bloodstream. | |
| Local anesthetic toxicity | Signs and symptoms of local anesthetic toxicity include:
|
Clamp the tubing and call the Acute Pain Service immediately. |
| Local anesthetic toxicity | Emergency signs and symptoms of local anesthetic toxicity:
|
Clamp the tubing and call 9-1-1 immediately. |
| Dressing | Leaking: if enough fluid is leaking that it is dripping out of the dressing AND your child's pain has increased. | Dry the skin and reinforce the dressing if it is lifting. Notify the Acute Pain Service if fluid is leaking out of the dressing. |
| Dressing | Edges of the dressing are lifting | Reinforce the edges with new dressing or tape. |
| Dressing | The dressing has fallen off | Apply a new dressing and notify the Acute Pain Service. |
| Elastomeric device tubing | Tubing disconnects or breaks | Use the clamp provided in the take-home kit to clamp tubing between the break/disconnect and your child. Keep both ends of the tubing clean. Call the Acute Pain Service. |
| Pain | Your child has pain that is not well managed. | Ensure you are giving your child pain medications by mouth as instructed by your health-care team. Reposition and elevate the affected limb using pillows or blankets. If your child has done the above and is still having a lot of pain, call the Acute Pain Service. |
If your child is experiencing any of the complications or troubleshooting issues listed above you can call the Acute Pain Service 24 hours a day, 7 days a week using the contact information at the end of this article.
