What is a mole?
A mole, or nevus, is a very common skin growth. It occurs when the skin cells that make pigment, known as melanocytes, build up under the surface of the skin. Moles vary in size, colour and appearance. These can also change over time. They are usually round, but they may also have an oval or jagged shape. Many times, the colour of a mole depends on the person's skin tone. People with darker skin tend to have darker moles. Moles usually appear during childhood and adolescence. These tend to grow rapidly during periods of natural growth spurts.

Moles can be flat, bumpy or verrucous (like a wart). They usually occur in body parts that are frequently exposed to the sun, but they can be found anywhere, even on the scalp or genitals or inside the mouth or eyes.
Moles fall into two main groups:
- congenital melanocytic nevi – moles that your child has at birth or are noticed shortly after birth
- acquired nevi – moles that develop later in life
How do moles affect the body?
Moles are usually benign (harmless). They can sometimes change and become skin cancer (melanoma). This can be very serious and sometimes lead to death if not treated in time. This is very rare in children.
Benign moles
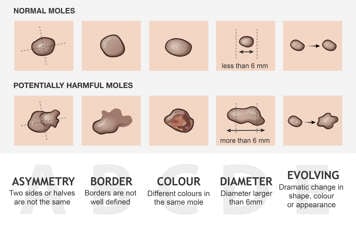
A benign mole often has the following three features.
- It is symmetrical – you can draw an imaginary line and divide it into two identical pieces.
- It has a regular border – there is a clear difference between the colour of the mole and skin around it. You clearly see where it starts and where it ends.
- It has a uniform pigment – every area of the mole is the same colour.
In general, benign moles:
- grow as your child grows, becoming bigger as the skin stretches
- may get darker or lighter with time
- may sometimes have coarse hair growing from them
- will normally change a little throughout life; for example, they may become raised over several years
Potentially harmful moles
A mole that is potentially harmful might:
- change shape
- rapidly grow (out of proportion with the child’s growth)
- develop an uneven colour
- form a scab or bleed without any injury
A dermatologist (skin specialist) should examine your child’s skin if it looks different than it used to, if an area opens up, bleeds and has a hard time healing or if a new mole suddenly appears and grows rapidly.
What causes moles to appear?
Several factors can cause moles to appear:
- genetic factors (children of parents with moles are more likely to also have moles)
- having fair skin and light hair, particularly red hair
- sun exposure (more time in the sun increases the number of moles on your skin)
- higher levels of cortisone, corticotropin and other hormones that help the body grow
- receiving growth hormone
- chemotherapy (medication that treats cancer)
- radiation therapy (used in some cancers)
- immunosuppression (a weakened immune system that prevents the body from fighting infections).
Can children develop melanoma?
Yes, they can. Although, melanoma in children is very rare. Only one child in one million children below age 15 develops melanoma.
The risk factors for developing melanoma during childhood include:
- having dysplastic nevi (irregular looking moles)
- having a close family member, such as a parent or grandparent, with a history of melanoma
- having a large number of melanocytic nevi, or moles (more than 50)
- being immunosuppressed or having an immunodeficiency (weakened immune system)
- having a sun-sensitive phenotype (very fair skin, light-coloured eyes and red or light hair)
- being exposed to ultraviolet radiation from the sun
- having a history of malignancy (any form of cancer)
- having a genetic disorder that makes the skin more sensitive to sun damage (for example, xeroderma pigmentosum)
How is a potentially harmful mole diagnosed?
Children with multiple moles tend to have moles with similar appearances. If a mole appears different than the rest of the moles on your child's skin, it may be a potentially harmful mole. This is known as the "ugly duckling" sign.
Dermatologists and other health-care professionals use the letters "ABCDE" as a guide when checking the skin for potentially harmful changes in existing or new moles. You can also use this guide when checking your child’s skin at home.
- A stands for asymmetry (having two sides or halves that are not the same).
- B stands for border irregularity (the borders of the mole are not well defined).
- C stands for colour variation (different colour tones in the same mole, for example light and dark brown).
- D stands for diameter larger than 6 mm.
-
E stands for evolving (including any dramatic change in shape, colour or appearance in existing moles).
In children, the use of "ABCDE" criteria as above might miss some potentially harmful moles. Using a modified "ABDC" with the traditional "ABCDE" may help to better identify potentially harmful moles in children.
- A stands for amelanotic (not pigmented).
- B stands for bumps or bleeding.
- C stands for uniform colour.
- D stands for variable diameter or de novo (new) development.
If a mole has any of these characteristics, it should be examined more closely. A dermatoscopic examination (examining the skin using a special magnifying glass) or a
skin biopsy (examining a small sample of the mole’s cells under a microscope) can tell your dermatologist or doctor if the mole is benign or malignant.
What can I do to reduce the risk of melanoma?
-
Avoid too much sun exposure (use a hat, seek shade, use a wide rim hat and use sun protective clothing (special SPF clothing) at the beach or in sunny places). Having sunburns in childhood increases the likelihood of developing skin cancers later in life.
- Do not let your child or teenager use tanning beds.
- Use sunscreen (SPF 30 or higher, covering both UVA and UVB rays) every day, even during winter months, and reapply it periodically during the day.
- Check the skin using the ABCDE abbreviation at least once every six months.
- Talk to your child’s doctor if you notice any change that concerns you.
How can I or my child inspect my child’s skin at home?
- Do the inspection in a well-lit area.
- If you are inspecting your child’s skin, gather a hair dryer, two chairs or stools, a camera or smartphone, a ruler and a pen and paper. If your child is inspecting their own skin, they will need these tools and two mirrors, one that is a hand-held mirror and one hanging on a wall or a door.
- Inspect the different parts of the body in the same order each time. For example, always work from the head down or the feet up.
- If working down from the head, for example, start by parting your child’s hair with a hair dryer or your hands to check their scalp. This is easier to do when the hair is wet.
- Check your child’s shoulders, chest and genital area.
- Check the back of their shoulders, their upper and lower back and their buttocks.
- Check their upper arms, elbows, forearms, wrists, hands, palms and fingers, including the space between their fingers.
- Check their inner and outer legs, front and back, including their knees and ankles.
- Check their feet and toes, including the soles and the space between the toes.
- Take a photo of any moles with a ruler beside them so you can record the size and keep track of any changes over time.
