What is hypopituitarism?
Hormones are chemicals produced in the body. They act as messengers that travel to other parts of the body where they affect how organs work. Hypopituitarism is a condition where the pituitary gland does not produce one or more pituitary hormones, or it does not produce enough hormones. "Hypo" means less than usual. The term "panhypopituitarism" means many or all of these hormones are deficient ("pan" means all).

The pituitary is a pea-sized gland located in the middle of the skull. It is part of the body’s endocrine system, which includes all the glands that produce and regulate hormones. The pituitary gland acts as the control centre for other glands. Hormones produced in the pituitary gland impact many other parts of the body. The pituitary releases various hormones in response to chemical messages it receives from the part of the brain called the hypothalamus.
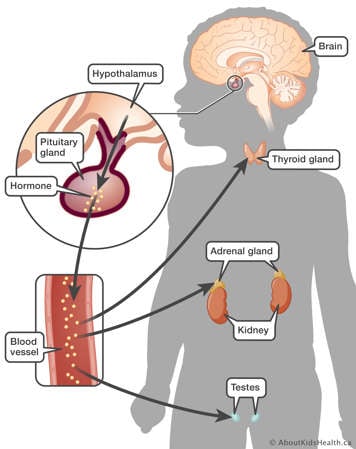
The target glands are those glands in the body that make their own hormones in response to hormones received from the pituitary gland. Some of these target glands include:
- the thyroid gland
- the adrenal gland
- the ovaries in females and the testes (or testicles) in males
Once the hormones are released from the target glands, the bloodstream then carries them to the tissues and organs of the body that use them. For example, hormones produced in the thyroid impact the body’s metabolism, heart rate, temperature, and more.
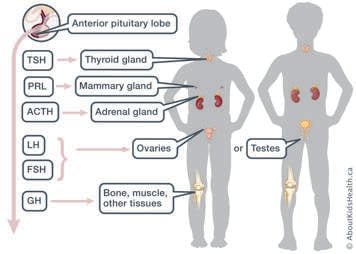
The front (anterior) part of the pituitary gland produces several different types of hormones that are needed for the body to function normally. The hormones that come from the anterior pituitary gland are:
- thyroid stimulating hormone (TSH)
- prolactin (PRL)
- adrenocorticotrophic hormone (ACTH)
- luteinizing hormone (LH)
- follicle stimulating hormone (FSH)
- growth hormone (GH)
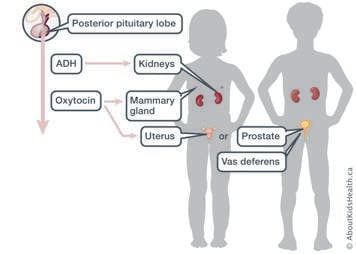
The back (posterior) part of the pituitary stores the hormones known as antidiuretic hormone (ADH) and oxytocin.
What causes hypopituitarism?
In many cases, the cause of hypopituitarism is unknown. However, it is not generally something that is passed on by parents to their children. Hypopituitarism may be:
- Congenital (meaning present at birth) – The pituitary or hypothalamus did not form normally before birth (e.g., septo optic dysplasia).
- Acquired – There was damage to the pituitary or hypothalamus during or sometime after birth.
A tumour in the pituitary area of the brain, a severe head injury, or a brain infection (such as encephalitis) can result in acquired hypopituitarism. Other causes include surgical removal of the pituitary gland, some chemotherapy, or radiation therapy to the part of the brain where the pituitary is located.
What hypopituitarism means to you
At this time, your child may be missing one or more pituitary hormones. As a result, it is important for you and your family to have knowledge of ALL the other pituitary hormones, because sometimes children have evolving hypopituitarism (loss of more pituitary hormones over time). Your child’s doctors and nurses will watch for signs and symptoms of additional hormone deficiencies whenever you are seen in clinic. However, we also rely on your observations between visits. Hypopituitarism is almost always a permanent condition, but it is treatable. Treatment involves replacing the hormones normally made by the target glands with hormones your child takes as a pill, injection (needle), or intranasal (in the nose) spray. We will review each hormone separately, and its effect on growth, development, and continued good health.
Different types of hormone deficiencies
Hypopituitarism may include the following hormone deficiencies:
- Growth hormone (GH) deficiency. GH affects the growth of bone, muscle, and other body tissues.
- Gonadotropin (FSH, LH) deficiency. Gonadotropins begin the process of sexual development (puberty).
- Thyroid stimulating hormone (TSH) deficiency. TSH stimulates the thyroid to produce thyroid hormones, which are important for growth, physical development, brain development, and for normal metabolism of the body.
- Adrenocorticotrophic hormone (ACTH) deficiency. ACTH deficiency results in a lack of cortisol, which is a hormone made by the adrenal glands. Cortisol keeps the body’s blood sugar at a normal level and helps the body deal with physical stress, such as fever or injury.
- Antidiuretic hormone (ADH) deficiency. ADH helps the body to retain the water that it needs to function properly.
- Prolactin deficiency. Prolactin stimulates breast milk production after childbirth. Prolactin deficiency would not be noted or assessed until after a woman gives birth. There is currently no treatment for prolactin deficiency.
Infertility and hypopituitarism
For most people with hypopituitarism, just because the pituitary gland may not be fully functioning, it does not mean that the gonads (ovaries or testes) do not work. This will be monitored very closely. When a person with hypopituitarism is ready to have children, they should speak to their health-care provider to make sure their ovaries or testes are healthy. They may need to be referred to a fertility specialist.
Psychosocial impact of hypopituitarism
You may be faced with many challenges while taking care of a child with a chronic condition. Some challenges that families may face include:
- Learning and mastering new skills and knowledge to care for your child with hypopituitarism.
- Allowing time to accept the diagnosis.
- Financial challenges, particularly if medications are not covered by private insurance plans.
- Frequent clinic visits requiring time off work/school.
- Taking multiple medications and ensuring they are given on time.
- Finding a day care for a child with a chronic condition.
- Teasing or bullying, as children with hypopituitarism may be somewhat delayed as compared to their peers in the areas of growth (height) and development (puberty).
- Potential infertility or the need for assistive reproductive technologies in the future.
Parents/caregivers may feel guilty or blame themselves for their children’s health issues. It is important to remember that hypopituitarism is not a condition that can be prevented in any way. With a good understanding of hypopituitarism, correct hormone replacement and regular clinic visits, your child can look forward to a healthy life.
The following resources can also help you to support both your child and you:
- Living with a chronic condition: Overview
- Living with a chronic condition: Helping your child manage their health
- Living with a chronic condition: Maintaining your child's everyday routines
- Living with a chronic condition: Supporting yourself as a caregiver
Transitioning to adult care
The endocrine team will be there to help you and your child manage their hypopituitarism until they turn 18 years old. After that point, your child will be transitioned to an adult endocrinologist for ongoing follow up. For people who have evolving hypopituitarism, their adult endocrinologist may suggest yearly blood work to monitor pituitary function. Because of the complexity of hypopituitarism, having an involved and collaborative relationship with your adult endocrinologist very important.
For more information, please see the Transitioning to Adult Care Learning Hub: https://www.aboutkidshealth.ca/transitionadultcare.