The terms 'mother' and 'breastfeeding' are used throughout our documents; we recognize and respect that individuals and families may use other preferred terminology.
Breast changes after childbirth
Your breasts likely became tender and larger during pregnancy, as they prepared to make milk for your baby. Typically, within the first week after childbirth, you will feel further changes in your breasts as they start to produce more milk. These initial changes happen regardless of whether you are breastfeeding or not, due to hormonal changes that occur at delivery. After this stage, your breasts will continue to produce milk if you stimulate and empty the breasts on a regular basis. This demand and supply concept of breast milk production is maintained by breastfeeding your baby frequently. When your baby cannot breastfeed, you can maintain milk production by breast pumping. The following complications may occur while you are lactating, especially if your baby is not feeding effectively or you are not emptying your breasts often enough.
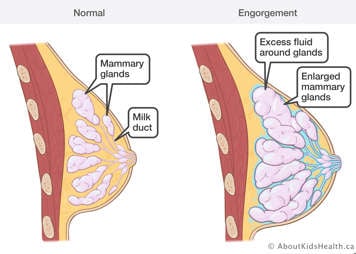
Breast engorgement
When your milk comes in between day three and five after birth, your breasts may become full, firm and uncomfortable. This is called breast engorgement. Engorgement is when there is swelling and increased pressure in the breasts due to an accumulation of breast milk and other fluid (interstitial fluid, lymph and blood).
Symptoms
- The whole breast feels hard, heavy and tight
- Breasts may have some redness and shine
- Tenderness
- Usually both breasts are affected
Causes
- The breast is not emptied for a long period of time
- The baby is not latching or drinking effectively
- It is part of the natural process of milk production in the first three to five days after delivery
Treatment
The most important strategy for relieving engorgement is frequent and effective milk removal from the breasts. You should breastfeed or breast pump at least eight times in 24 hours to help relieve engorgement and maintain your milk supply. Wear a well-fitted maternity bra for support.
Sometimes the swelling in the breast tissue during engorgement can be so severe that it stops the milk from flowing. It is important to treat this swelling as soon as it starts to occur:
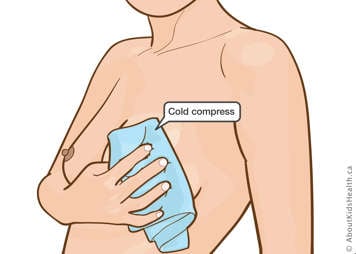
- Apply a cold compress to your breasts for 20 minutes after or in between breastfeeds or pumping sessions to reduce swelling.

- Only apply heat for a few minutes just before feeding or pumping if you are able to express some milk.

- Lie down and massage your breasts, pushing towards the arm pits.
- If needed, take an anti-inflammatory (such as ibuprofen) to control the pain and to reduce swelling.
Reverse pressure softening

If your areola (the dark area around your nipple) is swollen and this is interfering with milk flow and/or latching, you can do reverse pressure softening before feeding or pumping. You do this by placing the tips of your fingers on the areola and applying pressure for 60 seconds. This helps to soften the areola, which makes latching or pumping easier.
- It may be helpful to do this while lying down to help with fluid drainage.
- You can also refer to the International Breastfeeding Centre for more information on this technique.
- A lactation consultant can help you if you require assistance.
You may find hand expressing is also helpful to soften the areola enough for effective latching and pumping.
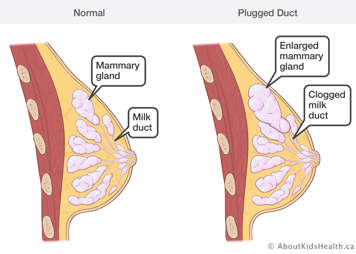
Plugged milk ducts
A plugged duct is an area in the breast that is not draining well, causing a blockage.
Symptoms
- Tender lump, or lumpy area in the breast—this is different from engorgement, as there is hardness in just one area of the breast
- Area may look red or feel warm
- Decreased milk flow from affected breast
- You otherwise feel well overall
Causes
- The baby is not latching well
- The baby is feeding less than usual due to illness
- Feeds or breast pumping sessions have been missed or shortened
- Tight restrictive clothing; wearing an underwire bra
- Sleeping on your tummy or more on one side
Treatment
The most important strategy for relieving a plugged duct is frequent and effective milk removal from the breasts. You should breastfeed or breast pump at least eight times in 24 hours.
A key element to treatment is removing the blockage to allow milk to flow. You can do this in the following ways:

- Apply heat (moist heat tends to work best).

- Massage in a circular or downward motion from behind the lumpy area towards the nipple.
- If breastfeeding, massage during the feed. Try breastfeeding in positions where the baby’s chin or nose are pointing towards the affected area.
- If pumping, massage during the pumping session.
- Try hand expressing after pumping to fully empty the breast.
- If needed, take an anti-inflammatory (such as ibuprofen) to control the pain and to reduce swelling.
- Wear the right sized bra (no underwire); loosen the bra to prevent compression of the milk ducts.
- Take care of yourself—rest, eat, drink.
A plugged duct can lead to mastitis. If symptoms do not resolve using the suggested treatments, seek medical attention.
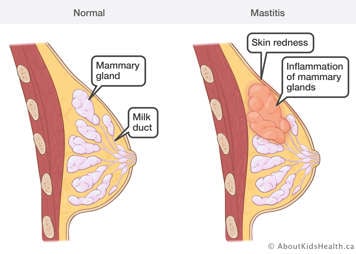
Mastitis
Mastitis is inflammation of the breast tissue, sometimes occurring with an infection.

Symptoms
- A red area on the breast—there can be red streaks
- Breast pain
- Flu-like symptoms such as fever, chills, fatigue, general aches and pains
- It usually affects only one breast
- Decreased milk supply on the affected side
Causes
- Inadequate emptying of the breast, caused by:
- Infrequent feeding or pumping
- Persistent engorgement or a plugged duct
- A poor latch
- Restricting feeding times
- An oversupply of milk
- Rapid weaning
- Other causes or risk factors are:
- Bacteria, often entering through a crack on the nipple
- Illness in the mother or infant
Treatment
The most important strategy for relieving mastitis is frequent and effective milk removal from the breasts. You should breastfeed or breast pump at least eight times in 24 hours.
Early mastitis with mild symptoms can be treated conservatively:
- Breastfeeding should be continued during this time. If your baby is not feeding at the breast, replace feeds with pumping until your baby returns to the breast.
- If breastfeeding, try different positions, including ones where the baby’s chin or nose are pointing towards the affected area.
- Your milk supply may drop significantly on the affected side, even with frequent emptying—try not to worry. Keep emptying your breasts, and your milk supply will likely return to normal once the mastitis clears.
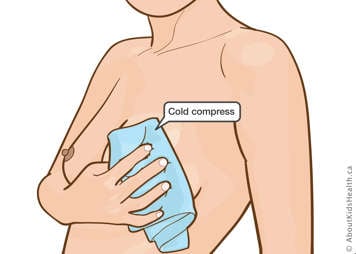
- Apply cold compresses for 20 minutes in between feeding or pumping to reduce pain and swelling.

- Place warm compresses on the affected breast for a few minutes before feeding or pumping to promote milk flow.

- Massage the blocked area in a circular or downward motion during pumping or feeding.
- If needed, take an anti-inflammatory such as ibuprofen.
- Take care of yourself—rest, eat, drink.
- Reach out for support to decrease stress and fatigue.
If you have a high fever, or if symptoms worsen or do not improve after 24 hours, seek medical attention immediately from your family doctor or closest emergency department: you may need antibiotics or further investigation of your symptoms.
Most antibiotics are safe with breastfeeding—discuss with your doctor, pharmacist, or call Health811 (811 | TTY: 1-866-797-0007).
Prevention
The best way to prevent breast complications while lactating is to empty the breasts frequently.
- If you are breastfeeding, feed on demand and ensure a good latch for effective milk removal.
- If you are pumping, pump both of your breasts at least eight times in 24 hours, and ensure proper flange fit and settings.
Hygiene:
- Wash hands frequently, especially if you have a crack or abrasion on your nipple or breast.
- Clean and sterilize your pump kits according to manufacturer instructions.
- Change breast pads frequently when wet, at least once a day.
Where to get help
All of these breast complications are associated with ineffective milk removal from the breast. It is strongly recommended that you see a lactation consultant as soon as difficulties arise to ensure the baby is feeding effectively, or for a pumping assessment.
You can also seek help from these other health-care professionals and resources, especially if mastitis is suspected:
- A family doctor
- An obstetrician or midwife
- A walk-in clinic
- Health811 (811 | TTY: 1-866-797-0007)
- An emergency department (for mastitis not responding to conservative treatment)

