The terms 'mother' and 'breastfeeding' are used throughout our documents; we recognize and respect that individuals and families may use other preferred terminology.
What does expressing breast milk mean?
Expressing breast milk, or pumping, is the removal of breast milk from your breast using a breast pump or your hands. You can then store your breast milk to give to your baby later.
You may need to express breast milk for one or more of the following reasons:
- To build up and maintain a milk supply when your baby in unable to exclusively breastfeed.
- To increase your milk supply.
- Your baby has a hard time latching (attaching) to the breast.
When is the ideal time to start expressing breast milk?
You should start to express your milk the day your baby is born, within six hours of birth. The first two weeks of your baby’s life are critical to establish your milk supply. The best way to express milk is to pump as instructed below.
What kind of pump should you use?
A hospital-grade, double electric pump is recommended to establish and maintain a breast milk supply. These electric pumps let you pump both breasts at the same time.
Breast pumps and kits are available at most hospitals: ask your nurse or lactation specialist. Many hospitals rent and/or sell the equipment needed for breast pumping at home.
Should you pump one breast after the other or both breasts at the same time?
It is better to express both breasts at the same time. This is called double pumping. Double pumping saves you time and helps to make more milk.
If you find double pumping difficult, purchase or make a hands-free pumping bra to help you.
How long should you pump at each pump session?
Pump for 15 minutes when you are double pumping. If you are single pumping, pump each breast for 15 minutes (for a total of 30 minutes). If your milk is still flowing, you can pump longer, up to 20 minutes. If you are pumping for twins, pump for 20 to 30 minutes.
How often should you pump?
You will need to pump your breasts every two to three hours, at least eight times a day, to make a full milk supply. This mimics how newborns feed (eight to 12 times in 24 hours), including overnight. You can have one longer period of four to five hours without pumping to sleep. If you sleep longer than five hours, your body can start to decrease milk production within two to three days. Remember, pumping sessions are timed from the start of one pump session to the beginning of the next.
Should you wait to pump until your breasts feel full?
This is a common question. It is true that if you wait longer between pump sessions you will get more milk at the beginning. However, the long time between pump sessions tells your body to decrease the amount of milk it is producing. More frequent pumping will tell your body to increase milk supply (see section called “What can you do to increase your milk supply?”). Track your milk volumes in a pump log, and focus on the 24-hour total volume of milk produced, instead of the volume at each pump session.
Why should you hand express breast milk?
Hand expressing after using a double electric breast pump can help you make more milk. You can hand express directly into the milk collection bottles provided by the hospital. Hand expression is especially important in the early days after your baby’s birth.
How to hand express breast milk
-

Hold your breast between your fingers and thumb, about 3 to 4 cm (1.5 inches) from the nipple (at the edge of the areola). Your finger and thumb should be opposite each other and in line with your nipple.
-

Keeping your fingers and thumb in place, press them back toward your chest wall.
-

Keep your fingers and thumb pressed back toward your chest wall. Now press them together, compressing the breast tissue between them.
-
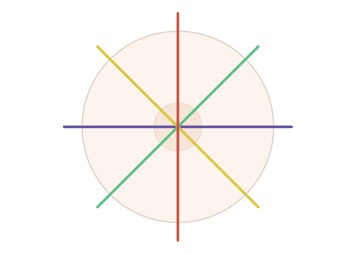
Continue this process until milk stops flowing. Then rotate your fingers and thumb to different positions around the breast (as shown by the coloured lines). Always keep your fingers and thumb in line with the nipple. You can go from one breast to the other.
How much milk should you expect to express?
In the first days after your baby’s birth, you may express no milk, a few drops or 5 to 10 mL of milk per session. Do not worry if you cannot express any milk in the first few days. Continue to pump and hand express at least eight times per day.
Breast milk production usually increases in volume two to four days after the birth of your baby.
| Premature baby | Term baby | |
|---|---|---|
| Age (in days) | 7 | 7 |
| Goal milk volume (in 24 hrs) | 350 mL | 500 mL |
| Age (in days) | 14 | 14 |
| Goal milk volume (in 24 hrs) | 750 mL | 750 mL |
Remember, any amount of breast milk is of benefit to your baby. Even if your milk volumes are low, keep going! Don’t give up. It may take time for your milk volume to increase. Speak to your lactation consultant or other health-care provider for additional support.
How can you keep track of your pumped milk volumes?
A pump log allows you to record how much milk you are making. Each time you pump your breasts, record the amount you pump and the time you started pumping. Keeping a record of your 24-hour volumes allows you to see increases and decreases in your milk volume.
A pump log can be downloaded and printed here: http://www.sickkids.ca/breastfeeding-program/Resources/72589-Pump%20Log.pdf.
You can also download a pump log app on your phone.
What can you do to prepare your breasts for pumping?
- You can put warm washcloths on your breasts or have a warm shower before pumping.
- You can massage your breasts before and during pumping to help milk flow.

Start at the outer edge of the breast. Massage the breast by making small circles, pressing into the breast tissue. Continue to massage in circles down toward the nipple.
Continue all the way around the breast.
There are many different methods of doing breast massage. Do what feels comfortable for you. For more information, see this instructional video: How to establish and maintain a breast milk supply for your hospitalized baby.
What should you do when you finish pumping?
- Take some of the breast milk and gently apply it to the nipple and areola. Allow the nipple to air dry. This helps keep the skin healthy.
- Place your breast milk in the sterile bottles provided.
- Remember to leave a half-inch space at the top of the bottle to allow the milk to expand when freezing.
- Use the labels provided by the hospital. Using a pen, write the time and date that you pumped on the label.
What can you do to increase your milk supply?
You can do something called “power pumping”, which is pumping every one to two hours for a period of time during the day. This mimics the cluster feeding pattern that babies go through during a growth spurt and tells your body to make more milk. When you first start pumping more often, you will likely get a lower volume of milk per pump session. However, over time, doing power pumping regularly for a few days will increase your milk supply.
When you are touching or holding your baby, the hormones that make breast milk increase. There are different ways to hold and touch your baby. Please see the video on Kangaroo Care at the following link for more information: http://www.sickkids.ca/breastfeeding-program/videos/index.html.
How do you know if the flange is the right size?
If your nipple rubs along the side of the tunnel, try a larger size. If your nipple is centred and moves freely, the fit is correct. If your nipple and an excessive area of your areola are pulled into the tunnel, try a smaller size.

Pumping should not be painful. If it is, speak to your lactation consultant or health-care provider for further assessment.
Will the cost of a breast pump be covered by insurance?
Some insurance plans will pay for the cost of a pump. Check with your insurance provider for more information.
How should you care for your breast pump kit at home?
If you are pumping for your hospitalized baby, after each pumping session you will need to:
- Rinse the pump kit parts with cold water
- Wash all the parts with hot soapy water
- Rinse all the parts well
- Dry all the parts with a paper towel, and store them in a clean, dry place
All the pump parts need to be sterilized according to the manufacturer’s instructions once a day. The tubing that attaches to the pump machine should not be submerged in water but may be wiped down with a disinfectant wipe.
How should you store your breast milk?
These guidelines are more conservative than those for healthy babies at home. We are being extra careful to protect your baby while in hospital.
Storing breast milk
| Where | How long |
|---|---|
| In the refrigerator | 2 days (48 hrs) |
| In the freezer unit of a fridge with two doors | 3 months |
| In a chest or deep freezer at -20°C (-4°F) | 6-12 months |
- Put your breast milk in the refrigerator right after pumping. If you are not going to use the milk within 24 hours, place it in the freezer.
- Once defrosted, breast milk must be used within 24 hours. Do not re-freeze milk that has been frozen and defrosted.
- Freshly pumped breast milk can be kept at room temperature for four hours if it does not come in contact with your baby’s saliva and is in a sealed container.
- Breast milk that has come in contact with your baby’s saliva can be kept at the bedside for one hour after it is warmed.
- Once the milk has passed the expiration time, throw it out.
How should you bring your breast milk to the hospital?
Bring your milk to the hospital in an insulated cooler with a frozen gel pack inside.
Do not add ice cubes to the cooler if the breast milk is frozen, as they will make the breast milk thaw faster.
For further information
Please visit www.sickkids.ca/breastfeeding-program/index.html, where you will find videos on expressing breast milk, kangaroo care, oral immune therapy, position and latch, breastfeeding intake assessment and breast complications.
