What is an arteriovenous malformation?

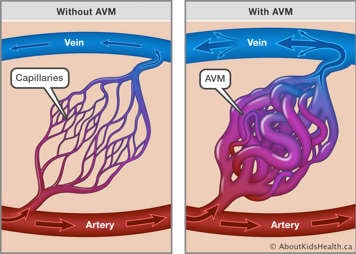
An arteriovenous malformation (AVM) is a complex tangle of abnormal blood vessels, where arteries are connected directly with veins without first flowing through normal capillaries. AVMs are most commonly found in the brain, but they can occur anywhere in the body.
Normally, blood circulates through the body from the heart through arteries, then into capillaries, then to veins, returning to the heart. Arteries have thick walls and carry blood that is under high pressure. Blood carried in arteries is rich with oxygen and nutrients as it is being pumped from the heart. Big arteries gradually get smaller. These then lead into the capillaries, which are small blood vessels where the exchange of oxygen, nutrients and waste happens. Blood flow slows down as it heads into the capillaries. Blood then enters the veins. Veins have thin walls and carry blood that is under low pressure, where the oxygen and nutrients have been used and waste products from tissues are returning to the heart to be replenished.
With an AVM, the high-flow artery blood enters the vein with a lot of pressure. Without the capillaries that gradually decrease the size of the vessels to help slow down the blood, high-pressure blood flows directly into the veins. The veins, which have weaker walls and are not used to the high-pressure, may stretch to the point of bursting.
Signs and symptoms of an arteriovenous malformation
A brain AVM may not cause any symptoms until it either increases in size or bursts.
Symptoms may include:
- headache
- seizure
- weakness, numbness or loss of movement in an arm, leg or one side of the body
- vision changes: loss of vision, seeing double, blurry vision, bothered by lights
- problems with speaking
- confusion
- sudden collapse
What are the causes of arteriovenous malformations?
The cause of brain AVM is unknown. AVMs are not typically present in the fetus or at birth, but it is believed that the genetic trigger exists in part of the affected blood vessels, leading to eventual development of the AVM later in life. Some AVMs can be associated with some genetic conditions such as hereditary hemorrhagic telangiectasia (HHT) and capillary malformation–arteriovenous malformation syndrome (CM-AVM). People with either HHT or CM-AVM were born with blood vessels (capillaries) that did not form properly. These blood vessels are fragile and prone to bursting/bleeding.
An AVM is rare and affects less than one percent of the population (10 per 100,000 people).
What may happen after an AVM is discovered?
A brain AVM can be detected in a scan that is being performed for a different medical reason, but it is usually discovered when there is bleeding inside the brain. When an AVM bursts and bleeds, there is an increased risk of another bleed happening in the next few weeks; so, it is very important that your child receives diagnostic imaging and treatment during this phase.
Diagnostic imaging and genetic testing
Diagnostic imaging is important in identifying an AVM. There are different types of imaging that can be performed to diagnose an AVM:
- Computed tomography (CT) scan: A CT scan uses X-rays and a computer to take “slice-like” pictures of the brain. Sometimes, further special CT imaging is done with contrast dye to take further pictures of the vessels of the brain. This is called a CT–Angiogram.
- Magnetic resonance imaging (MRI): An MRI uses a strong magnet to take a picture of the brain. The images of the arteries in the brain are called MRI–Angiograms (MRAs), and the images of the veins in the brain are called MRI – Venograms (MRVs). Sometimes, further special MRI imaging is done with contrast dye to take further pictures of the vessels of the brain.
- Cerebral angiogram: A cerebral angiogram uses medical imaging and contrast dye to create a map of the arteries so they can be seen by X-rays. It is the standard test for understanding all the unique details of an AVM.
Given that genetics may also play a role in the development of an AVM, your child’s health-care team may also discuss whether genetic testing is appropriate.
Medications
Medications may be used to treat some symptoms caused by an AVM, such as headaches or seizures. Future research will focus on identifying medications to treat brain AVMs directly based on their genetic make-up.
Treatment
The main goal of treating an AVM is to prevent bleeding/rebleeding. Treatment may also be discussed to control seizures or manage other symptoms.
There are three main treatment options for brain AVMs including open brain surgery (craniotomy), endovascular surgery (embolization) and stereotactic radiosurgery (Gamma Knife procedure). Some AVMs may require a combination of treatments.
Your child will be assessed by a group of neurovascular specialists, including neurosurgeons, interventional neuroradiologists, and stroke neurologists. Your child’s treatment recommendations will be made based on their age, health status, and the size and location of the brain AVM.
Open brain surgery (craniotomy and AVM removal)
Your child’s neurosurgeon will make an incision on the scalp and remove part of the skull bone temporarily to access the AVM. With special equipment, the AVM is located and carefully removed. The skull bone is then re-attached, and the incision is closed.
If your child’s AVM has burst, the goal of this surgery is to remove the blood clot. Your child will need time to recover from the bleed, including a period of rehabilitation therapy, before having additional treatment.
Endovascular embolization
Your child’s interventional neuroradiologist will insert a catheter into an artery in your child’s leg, wrist, or back of the hand, which is threaded through the blood vessels to the brain. Once the AVM is located, an embolizing agent (either coils or glue) is injected to block the artery and reduce blood flow to the AVM. This is often performed in the immediate period after a bleed to reduce the risk of re-bleeding. Embolization can also be performed as part of an open brain surgery or as a stand-alone treatment.
Stereotactic radiosurgery (Gamma Knife procedure)
Your child’s health-care team will use focused beams of radiation to damage and scar the AVM blood vessel walls, ultimately stopping the flow of blood to the AVM. The procedure delivers targeted doses of radiation therapy with the precision of less than one millimetre. Only the blood vessels being targeted receive a significant dose of radiation, while the surrounding brain tissue remains unharmed. Stereotactic radiosurgery is used for areas of the brain where surgery would be too difficult or too dangerous.
What are common complications of arteriovenous malformations?
- An AVM can grow in size, putting pressure on the brain that is around it.
- An AVM can steal blood from areas of the brain around it, causing scarring of the brain called gliosis.
- An AVM can burst and bleed into the surrounding brain and cause damage and risk to life.
The risk of a brain AVM bleeding is around 2-4 % each year, and the lifetime risk of bleeding can be quite high, more so in children and young adults. The risk of bleeding is higher in AVMs that have previously bled.
Brain injury from a brain AVM bleeding may be potentially life-threatening or cause significant disability. An urgent open brain surgery may be needed depending on the location of the bleeding, the amount of blood and the amount of pressure the brain is under.
AVMs can also have large connections between arteries and veins (fistulas) or bulging or ballooning areas in vessel walls (aneurysms) as part of the malformation.
Helping your child
Receiving the diagnosis of an AVM can be very stressful and emotional. Your child’s health-care team can suggest resources that may be available for you and/or your child to help to with coping.
For more information on coping, see:
- Living with a chronic condition: Overview
- Living with a chronic condition: Helping your child manage their health
- Living with a chronic condition: Maintaining your child's everyday routines
- Living with a chronic condition: Supporting yourself as a caregiver
- Mental health learning hub
- Guided audio meditations
- Mental health animations for kids and teens
Follow-up care
Your child will require several years of follow-up care and imaging to ensure that the AVM has been treated and there is no evidence of it coming back.
When to seek medical attention
It is important to take your child to the nearest Emergency Department if they experience any of the following symptoms:
- Headache
- Seizure
- Weakness, numbness or loss of movement in an arm, leg or one side of body
- Vision loss
- Problems with speaking
- Confusion
- Sudden collapse
At SickKids
SickKids Neurosurgery Clinic – SickKids Neurosurgery offers the highest level of care to children with all types of neurosurgical disorders.
Paediatric Neurovascular Program – The Paediatric Neurovascular Program is made up of a team of specialists dedicated to providing care to children with neurovascular diseases.
References
Berman MF, Sciacca RR, Pile-Spellman J, Stapf C, Connolly ES Jr, Mohr JP, Young WL. The epidemiology of brain arteriovenous malformations. Neurosurgery. 2000 Aug;47(2):389-96; discussion 397. doi: 10.1097/00006123-200008000-00023. PMID: 10942012.
Pollock BE, Flickinger JC, Lunsford LD, Bissonette DJ, Kondziolka D. Factors that predict the bleeding risk of cerebral arteriovenous malformations. Stroke. 1996 Jan;27(1):1-6. doi: 10.1161/01.STR.27.1.1.