There are no effective medicines for hydrocephalus, and most children require surgery. The goal is to lessen the pressure in the brain by providing another pathway for cerebrospinal fluid (CSF) to be drained and absorbed away from the brain.
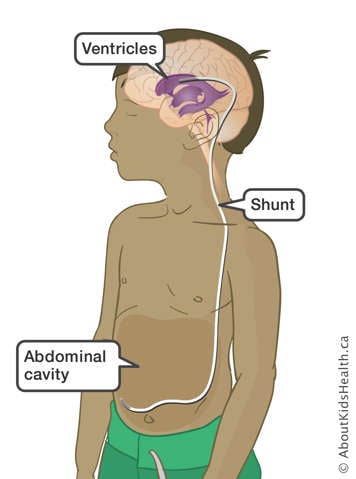
The most common treatment for hydrocephalus is the insertion of a shunt. The shunt works by moving fluid from an area where there is too much CSF to an area where it can be absorbed into the body.
Shunt surgery
The most common treatment of hydrocephalus is the surgical placement of a shunt. A shunt is a soft, flexible tube.
The top end of the shunt is placed in the ventricle fluid spaces inside the brain. This tube is attached to a valve that controls the flow of CSF through the shunt. The tube is then tunnelled below the skin to an area of the body where the fluid can be absorbed. One area is the lining of the abdominal cavity (the peritoneum). This is called a ventriculo-peritoneal shunt (VP shunt).
Less often, the shunt is connected from the brain to other parts of the body:
- A shunt from the brain to the lining around the lung (pleural space) inside the chest is called a ventriculo-pleural shunt.
- A shunt from the brain to veins draining into the heart is called a ventriculo-atrial shunt.
There are different types of shunt tubes and valves
Your child's neurosurgeon will decide what type of shunt tube is best for your child. All shunts will only allow CSF flow in one direction. Some shunts may also have a small bubble or "reservoir" near the top that a health-care provider can use to take samples of CSF for testing.
Sometimes, a special type of shunt is needed where the pressure setting is adjustable. This is called a programmable shunt valve. This allows your child’s health-care provider to program the shunt to control how much CSF is draining. It is important to remember that the pressure setting of this shunt can be changed by a magnet. Magnetic resonance imaging (MRI) scans use large magnets; so, if your child needs an MRI, you must make sure to tell their health-care provider about the shunt. After an MRI, a programmable shunt valve needs to be checked to make sure that the pressure setting has not been changed.
Preparing for the procedure
Most parents and children are more comfortable with their visit to the hospital if they know what will happen when they arrive. Please see Coming for surgery to find out how you can prepare your child for their shunt surgery.
If you have any specific questions about your child’s procedure before their surgery, contact your child’s neurosurgery team.
During the shunt operation
Your child will be brought down to the operating room and go to sleep under general anesthesia. Your child will not feel any pain during the operation.
The area from the head to the abdomen (belly) or chest (depending on where the end of the shunt is going), will be scrubbed with an antiseptic soap. The neurosurgeon will make incisions (cuts) on your child’s head and abdomen or chest, depending on the type of shunt. The shunt tubing will be tunnelled just below the skin. The ventricular (top) end of the shunt is then passed through a small hole in the skull made by the neurosurgeon and gently passed into the ventricle. The abdominal or chest (bottom) end will be passed through a small opening in the abdomen or chest. The incisions are then closed using staples or stitches.
The operation will take between one and two hours.
After the shunt operation
- Your child will wake up soon after the operation. You will be able to see your child after they wake up.
- Your child will have a bandage on their head and another bandage on their abdomen or chest, depending on the type of shunt.
- A nurse will check on your child often. They will also be checking to see how easily your child wakes up, even at night.
- Your child will have an intravenous (IV) line after surgery until they are able to drink well.
- Your child may have a computed tomography (CT) or MRI scan after surgery to make sure the ventricles have decreased in size and that the shunt is in a good position.
Pain after the operation
After the operation, your child may have pain at the operative sites. A nurse will give your child medicine as needed to control the pain. If it does not control the pain, speak to your child's health-care team.
Your child may also learn other ways to control pain, such as blowing bubbles or relaxation breathing. Ask your child’s health-care team to help you and your child learn how to do this.
Your child's health-care team will tell you when your child can start normal activity, such as sitting up and walking. After your child has recovered from the surgery, they can go home.
Going home after the operation
When a child has a shunt, there is always a risk that a problem with the shunt could develop in the future. Sometimes, the tube can become blocked, come apart, or break. The tube may also move out of the abdomen as your child grows, if they have received a VP shunt. The shunt may also become infected.
Following up after the operation
Your child’s neurosurgeon will need to see your child for a follow-up clinic visit about six weeks after you go home. The appointment may be made for you when your child leaves the hospital. If one has not been made, call the neurosurgery clinic to make an appointment when you get home.
Any medical questions you may have after the procedure can be answered by your child’s health-care team at their follow-up appointment. Be sure to write down your questions beforehand.
Removing staples or stitches
How your child's staples or stitches are taken out depends on the type of staple or stitch that was used. Your child’s health-care team will tell you whether staples or stitches were used.
- If your child has staples or stitches that need to be taken out, this can often be done by their primary health-care provider. The stitches should be taken out about seven to 10 days after the operation. Staples should be removed about 10 days after the operation. Your child’s health-care team will confirm when they need to come out.
- If staples were used, you will be given a special remover to take to your child’s primary health-care provider.
- If your child has the kind of stitches that dissolve on their own, you can see your child’s primary health-care provider to have the incision line checked; but the stitches will not need to be removed.
Longer-term: as your child grows to adulthood
A child with hydrocephalus needs to see the neurosurgery team often to make sure the shunt is working properly and that the pressure does not begin to build up again. Several members of the team will help and guide you as your child grows and develops. You should encourage your child to become involved in this ongoing process.
When to seek medical attention
If you notice any signs of a shunt problem or hydrocephalus symptoms coming back, it is very important to seek medical attention right away. Call 911 or go to the closest Emergency Department.
Possible signs that the shunt is not working
In babies, the following signs and symptoms may occur:
- poor feeding
- vomiting (throwing up)
- sleepy (hard to wake up) or not as awake or alert as usual
- large head (your child’s primary health-care provider can measure this)
- bulging soft spot (fontanelle) on the top of the head
- seeming irritable (cries easily or without reason)
- seizures
- very noticeable scalp veins
- slowness at reaching milestones (for example, slow to roll over, slow to sit) or loss of milestones (for example, was sitting or walking and now unable)
- "sunset" eyes, when the eyes appear to be always looking down and are not able to look up
In older children, the following signs and symptoms may occur:
- headaches
- nausea and vomiting
- tired (sleeping more than usual, difficult to wake up, does not want to play as usual)
- seeming irritable
- changes in personality, behaviour or school performance
- loss of coordination
- seizures
- changes in vision
Shunt malfunctions and infections
Shunt malfunctions and infections that are not treated promptly and appropriately can lead to serious consequences.
Signs of a shunt infection can include the following:
- puffiness or redness of the skin around the tube and at the incision (cut) sites
- a fever
- a stiff neck
- fluid coming out of the incision sites
- loss of appetite or not eating well
- generally feeling sick
- headache
- abdominal (belly) pain or chest pain, depending on the location of the shunt
To learn more about the signs and symptoms that would indicate your child's shunt is not working properly, see Shunt revisions.
To learn more about what to do if your child’s shunt becomes infected, see Shunt infections.
At SickKids
The Neurosurgery unit is located on 5C, 5th floor of the Atrium.
The Neurosurgery clinic is located on 6C, 6th floor of the Atrium. Phone: 416-813-5222.