What is intra-arterial chemotherapy?
Intra-arterial chemotherapy (IAC) is a procedure for the treatment of retinoblastoma, which is a cancer that forms in the retina at the very back part of the eye. IAC is performed by a pediatric neurointerventionist—a doctor that performs brain vessel procedures in children.
About intra-arterial chemotherapy
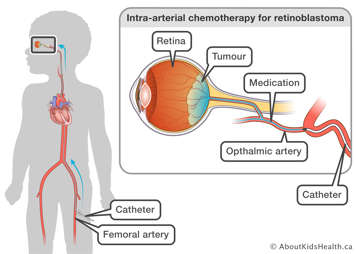
During the procedure, chemotherapy medications are delivered directly to the tumour by a small flexible tube called a catheter that is inserted through the femoral artery (groin) under image guidance and directed to the artery of the eye. A special dye, called contrast, and X-rays are used to see the blood vessels inside your child’s body and to make sure the catheter is in the right place. IAC allows for a very small dose of strong chemotherapy medications to be directly injected into the eye with very few side effects.
The ophthalmology team will usually examine your child while your child is under anesthesia after the procedure to gauge the effects of treatment. The findings will be discussed with the neurointerventionist and communicated with you.
When the procedure is finished, the catheter is removed, and pressure is applied to the groin to stop any bleeding. There will be a small clear dressing at the insertion site after the procedure.
Typically, most children require 2-4 cycles of IAC. Each cycle is 3-4 weeks apart. Each IAC treatment will take between 2-3 hours to complete. The procedure is done as a day procedure and does not require admission to the hospital.
Risks of the intra-arterial chemotherapy
IAC is usually a low-risk procedure. Major complications from IAC are rare and are similar to the risks of any brain vessel procedure. Some of these are listed below. The neurointerventionalist will discuss these with you during your child’s consultation appointment.
During the procedure:
- Clotting (blockage) of the arteries
- Damage to the arteries examined (dissection, rupture, bleeding, blockage)
- Allergy to X-ray contrast dye
- Reduced function of organ and tissue (stroke, paralysis, vision loss)
- Change of heart rhythm and breathing
Immediately after the procedure:
- Pain, bruising or bleeding in the groin where the catheter was inserted
- Poor circulation to the leg or arm where the catheter was inserted
The first week after the procedure:
- Swelling in the eyelid of the treated eye
- Thinning of the eyebrows and lashes
- A bulge or weakness in the artery wall (pseudoaneurysm) in the groin where the catheter was inserted
Visiting the clinic before the procedure
Your child may have a clinic visit with the neurointerventionist before the procedure. During the visit, you should expect:
- A health assessment to make sure your child is healthy, and that it is safe to have general anaesthesia and to go ahead with the procedure.
- An overview of the procedure and a review of the consent form.
- Blood work, if needed.
Giving consent before the procedure
Before the procedure, the neurointerventionist will go over how and why the procedure is done, as well as the potential benefits and risks. They will also discuss what will be done to reduce these risks and will help you weigh benefits against the risks. It is important that you understand all potential risks and benefits of the procedure and that all of your questions are answered. If you agree to the procedure, you can give consent by signing the consent form. The procedure will not be done unless you give your consent.
How to prepare your child for the procedure
Before any treatment, it is important to talk to your child about what will happen. When talking to your child, use words they can understand. Let your child know that medicines will be given to make them feel comfortable during the procedure.
Children feel less anxious and scared when they know what to expect. Children also feel less worried when they see their parents are calm and supportive.
If your child becomes ill within two days before the procedure
It is important that your child is healthy on the day of their procedure. If your child starts to feel unwell or has a fever within two days before the procedure, let your ophthalmologist or oncologist know. Your child’s procedure may need to be rebooked.
Food, drink and medicines before the procedure
- Your child’s stomach must be empty before general anaesthetic.
- If your child has special needs during fasting, talk to your doctor to make a plan.
- Your child can take their regular morning medicines with a sip of water up to two hours before the procedure.
- Medicines such as acetylsalicylic acid (ASA), naproxen or ibuprofen, warfarin, or enoxaparin may increase the risk of bleeding. If your child is on any of these medications, consult with your child’s oncologist and neurointerventionist before the procedure to create a plan of care.
On the day of intra-arterial chemotherapy
Arrive at the hospital two hours before the planned time of your child’s procedure. Once you are checked in, your child will be dressed in a hospital gown, weighed and assessed by a nurse. You will also be able to speak to the neurointerventionist and the anesthesiologist who will be giving your child medication to make them comfortable during the procedure.
During the procedure, you will be asked to wait in the surgical waiting area.
Your child will have medicine for pain
Children are given medicine for treatments that may be frightening, uncomfortable or painful. For IAC, children are given general anaesthesia to reduce movement and to control their heart rate and blood pressure. They are also given local anaesthesia at the groin where the catheter is inserted to make sure they are comfortable.
After the procedure
Once the IAC is complete, your child will be moved to the recovery area. The neurointerventionist will update you about the details of the procedure. As soon as your child starts to wake up, a nurse will come and get you.
After the procedure, your child should remain lying down on their back with their leg kept straight for four hours. Some sedation medication will be prescribed for the first hour. If there is any oozing or bleeding from the insertion site at the groin, some pressure may be applied. Slow walking and movement can begin after four hours if there are no concerns at the accessed groin site. For smaller children who need to be picked up to feed, this can be done after two hours if there are no bleeding concerns at the groin.
Going home
In most cases, children go home the same day as the procedure. This usually occurs about six hours after the procedure. Your child’s nurse will let you know when they are well enough to go home.
For more details on how to care for your child after IAC, please see Intra-arterial chemotherapy for retinoblastoma: Caring for your child at home after the procedure.
At SickKids
If you have any concerns in the first 48 hours after the procedure, call the Image Guided Therapy (IGT) clinic at (416) 813- 7654 ext. 201804. Speak to the IGT clinic nurse during working hours or leave a non-urgent message.
If you have concerns and it is after working hours, see your primary care provider or go to the nearest Emergency Department. You can also call the Hospital for Sick Children switchboard at (416) 813-7500 and ask them to page a member of your child’s health-care team or the interventional radiology fellow on call.
For more information on fasting see Eating and drinking before surgery.
For more information on preparing your child for their procedure see Coming for surgery.