What is a port?
A port is a special intravenous (IV) line that is placed completely inside the body.
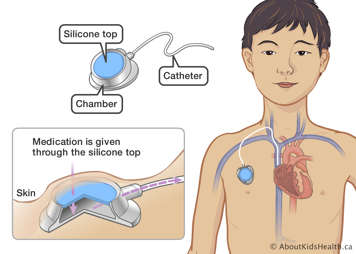
A port consists of two parts:
- The first part is the port itself. This is a small chamber made of metal, with a soft silicone top. It lies just under your child’s skin. Your child will receive IV therapy by having a needle inserted through the skin into the port.
- The second part is a long, soft, thin, flexible tube called a catheter. One end of the catheter is attached to the port and the other end is inserted into one of the large veins that leads to the heart.
The port and the catheter allow medicine to be delivered directly into the blood.
Why is a port inserted?
A port is used in some children who need IV therapy for a long period of time. IV therapy can include medications such as chemotherapy, and IV nutrition and fluids. Your child may also need a port because there are some medications that cannot be given through a regular IV line. Having a port inserted makes it easier and more comfortable for your child to receive these IV therapies. If your child has a port inserted to receive IV therapies then it can also be used to take blood samples.
How is a port inserted?
A port is inserted using image guidance by an interventional radiologist. During the procedure, the tip of the catheter is inserted into a vein in the neck with the assistance of ultrasound or a special kind of X-ray called fluoroscopy. The catheter is guided through the veins until it is positioned in the large vein just above the heart, where blood flow is fast.
The other end of the catheter is tunneled under the skin a short distance to a space called the pocket, which is created by a small incision. The pocket is where the port sits, under the skin. The tissue and skin are then stitched closed. The stitches used will dissolve and do not require removal.
A chest X-ray may be taken after the procedure to make sure the port is in the correct position.
It will take about one to 1.5 hours to insert the port.
Risks of a port insertion for your child
A port insertion is usually considered a low-risk procedure. The risks of the procedure will vary depending on your child’s condition, age and health.
The risks of a port insertion include:
- failure to find an open vein that will accept the port catheter
- bleeding or bruising
- pain or discomfort
- infection
- clotting
- air in the lungs or veins
- irregular heart rhythm
- breakage of the catheter
- movement of the catheter
- X-ray exposure
- vein perforations
- nerve or artery damage
Preparing for a port insertion
If your child is already in the hospital, you will meet a nurse from the Vascular Access Service who will explain the procedure and answer your questions. If your child is an outpatient, the health-care team looking after your child will explain the procedure to you.
Giving consent before the procedure
Before the procedure, a member of the interventional radiology team will go over how and why the procedure is done, as well as the potential benefits and risks. They will also discuss what will be done to reduce these risks and will help you weigh the benefits against them. It is important that you understand all of these potential risks and benefits of the port insertion and that all of your questions are answered. If you agree to the procedure, you can give consent for treatment by signing the consent form. A parent or legal guardian must sign the consent form for young children. The procedure will not be done unless you give your consent.
How to prepare your child for the procedure
Before any treatment, it is important to talk to your child about what will happen. When talking to your child, use words they can understand. Let your child know that medicines will be given to make them feel comfortable during the procedure.
Children feel less anxious and scared when they know what to expect. Children also feel less worried when they see their parents are calm and supportive.
Food, drink, and medicines before the procedure
- Your child’s stomach must be empty prior and during general anaesthetic.
- If your child has special needs during fasting, talk to your doctor to make a plan.
- Your child can take their regular morning medicine with a sip of water two hours before the procedure.
Medicines such as acetylsalicylic acid (ASA), naproxen or ibuprofen, warfarin, or enoxaparin may increase the risk of bleeding. Do not give these to your child before the procedure unless they have been cleared first by your child’s doctor and the interventional radiologist.
On the day of the port insertion
Your child will have medicine for pain
It is important that your child is as comfortable as possible for the procedure. Your child will receive a general anaesthetic for the port insertion, so they will not hear or feel anything during the procedure.
During the port insertion, you will be asked to wait in the waiting area.
After the port insertion
Once the port is inserted, your child will be moved to the recovery area. The interventional radiologist will come and talk to you about the details of the procedure. As soon as your child starts to wake up, a nurse will come and get you.
How long can the port stay in?
A port can stay in for months or years, as long as it remains problem-free and working well.
Removing the port
Once your child's health-care team is confident that the port is no longer needed, they will make arrangements to have it removed. Ports are removed under general anaesthetic. This procedure takes about one hour. Eating and drinking restrictions are similar to when the port was inserted.
At SickKids
At SickKids, the interventional radiologists work in the Department of Diagnostic Imaging – Division of Image Guided Therapy (IGT). You can call and speak to the Vascular Access Service resource nurse at (416) 813-6986 during working hours, or leave a message with the Vascular Access Team. If you have concerns and it is after working hours, please call the Hospital for Sick Children switchboard at 416-813-7500 and ask them to page your child’s doctor on call, or go to the nearest Emergency Department.
For more information on fasting, see “Eating and drinking before surgery.”
For more information on preparing your child for their procedure, see “Coming for surgery.”
Additional resources
Seek the care of a health-care professional if you have any questions regarding SPARK Care Recommendations or your child’s diagnosis or symptoms.


