Cancer pain
Cancer pain may be related to the disease itself or as a side-effect of treatment such as radiotherapy and chemotherapy. Cancer pain can be either nociceptive or neuropathic, or a combination of both. It can be acute or chronic. If it has become life-threatening it may require the services of a palliative care team.
Palliative pain
Palliative care begins with the diagnosis of a progressive, life-threatening condition. It is the active total care of the child’s body, mind, and spirit. It also involves giving support to the family. The goals of palliative care are to provide optimal comfort and quality of life, and to sustain hope and family connection despite the likelihood of death. Paediatric palliative care aims to provide comprehensive care for children and their families through the living, dying, and grieving processes. It affirms life and regards dying as a process that is a profoundly personal experience for the child and family. Control of pain, other symptoms, and psychological, social, and spiritual problems is paramount. Effective palliative care requires a broad multidisciplinary approach that includes child, family, and available community resources.
The assessment, treatment, and management of pain during the palliative phases of illness require vigilance on the part of health-care providers and the child’s family. The key is that for effective relief, treatments must target both the primary source of pain and its various secondary sources. There is no "ceiling" on the pharmacotherapy; the dosages will be increased, or titrated, until effective relief is achieved.
Recurrent pain
Recurrent pain is pain that comes and goes. Approximately 5% to 10% of schoolchildren will experience this at some point, most of whom will not seek treatment. The most common forms of recurrent pain are tension and migraine headaches, abdominal pain, and irritable bowel syndrome. Treatment often requires medication, psychological interventions, and physical interventions. The participation of the child is required to develop long-term coping strategies.
Procedural pain
Invasive procedures can be among the most painful and traumatic events experienced by children. Although procedure-related pain is usually short-lived, it is significantly different from acute pain caused by an injury. The child knows in advance that the pain is coming. Because the pain is anticipated, there is opportunity for fear and anxiety to build up before the procedure. Some children may experience anxiety-related symptoms such as nausea, vomiting, loss of appetite, skin rashes, insomnia, and nightmares. High levels of fear and anxiety can increase the intensity of the pain.
Although procedural pain creates an opportunity for fear and anxiety to build up and increase the pain experienced, also it provides an opportunity to do something about pain before the procedure starts. Pre-emptive steps can be taken to minimize pain before treatment begins. These protective or pre-emptive measures can include the use of drugs, physical measures such as rubbing or using ice, and psychological strategies such as distraction or blowing bubbles. The choice of which pain-relieving techniques to use depends on the type of procedure to be performed and the age of the child.
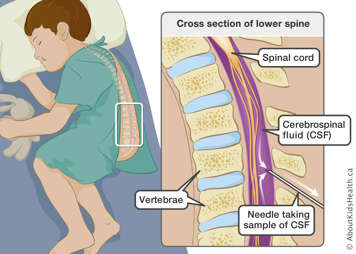
The most common painful procedures that children undergo include needle injection, lumbar puncture (spinal tap), and circumcision. Children with some types of cancer and other serious conditions may undergo other painful procedures such as bone marrow aspiration and biopsies.
If a child is receiving a vaccination, the pre-emptive pain relieving strategy might simply be to put some anaesthetic cream on the skin where the injection will take place about an hour before the needle is given. This will reduce the pain of the injection. In the case of more invasive and time-consuming procedures, a combination of medicines, distraction, and relaxation techniques may be used.
Without pre-emptive pain relief, children experience greater levels of anxiety with each repeat procedure. Moreover, the more uncomfortable the child is the longer and more difficult the procedures can become - which further increases anxiety. Imagine that a child does not want to get an injection because they know it will be painful. They may squirm and be generally uncooperative, which will lengthen the time necessary to give the injection and may compromise the safety and accuracy of the procedure.
Parents can help by being honest with their children about what is going to happen and by comforting them. Involving the child in the procedure and the pain relief is often helpful. Falsely telling a child that "this isn’t going to hurt" can increase the level of pain experienced by the child.
Some procedures do not allow for pre-emptive anaesthetic or analgesia. In most cases, this has to do with emergency situations. An injury can be so serious it must be treated immediately. Pain relief comes after the treatment.