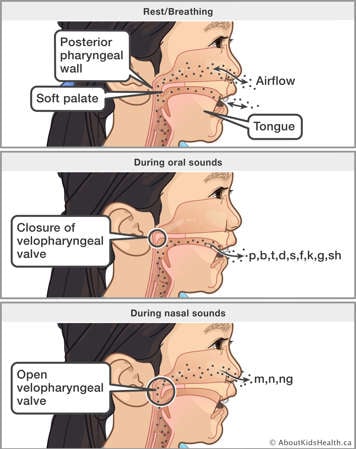
Nasal-sounding speech (hypernasality) occurs when too much air and sound escapes through the nose while talking. To prevent air and sound from passing through the nose while talking, the soft palate (velum) must rise up and touch the back wall of the throat (posterior pharyngeal wall). If there is not a complete seal, then air and sound can leak into the nose when it should not. When this occurs, it is called velopharyngeal dysfunction (VPD) or velopharyngeal inadequacy (VPI) and it results in hypernasal speech. When speaking English, velopharyngeal closure is needed for all sounds except for nasal sounds (m, n, ng).
Speech assessment
Children who are 3 to 4 years old are usually talking in short sentences and can provide a speech sample that can be evaluated for hypernasality.
A speech-language pathologist on the Cleft Lip and Palate Team will listen to the child's speech and decide whether it may be improved with therapy or whether more testing is needed.
The speech-language pathologist may use a computer test called the Nasometer to measure the amount of sound coming from the child's nose and mouth.
The muscles and structures of the velopharyngeal area during speech may also be tested using nasopharyngoscopy or multiview videofluoroscopy. Both tests involve the child repeating selected sounds, words and phrases. For nasopharyngoscopy, a small fiberoptic tube (endoscope) is inserted into one nostril to view the velopharyngeal area during speech . Multiview videofluoroscopy is an X-ray test that lets the speech-language pathologist see how the velopharyngeal area works during speech.
If testing shows the child's palate is not working properly (velopharyngeal dysfunction) and speech therapy alone will not correct the problem, then surgery may be recommended to improve speech.
After reviewing all the assessment results, the speech-language pathologist and the child's surgeon will discuss the treatment options with you and suggest the best one for your child.
A Furlow palatoplasty has been recommended for your child
A Furlow palatoplasty is an operation on the soft palate that lengthens the palate and corrects the position of the soft palate muscles. This helps the soft palate contact the posterior pharyngeal wall (back of the throat) to prevent air and sound from escaping through the nose during production of oral (mouth) sounds. This operation is chosen to correct hypernasal speech when the size of the velopharyngeal gap (space between the soft palate and back of the throat) is relatively small, or to repair a submucous cleft palate. The operation is done inside the mouth while the child is under general anesthesia.

Complete a pre-anesthesia assessment
The pre-anesthesia assessment is usually done as a phone call. A doctor or nurse practitioner will review your child's health issues and develop a plan for the anesthetic for the surgery. Some children may need to meet with an anesthesiologist before the surgery. You will be told which type of appointment your child needs.
Get your child ready
You play an important role in reducing your child's risk of infection by having them bathe using liquid soap before their operation.
Follow our feeding guidelines
Your child will be given a general anesthetic for the operation. This will help your child fall into a deep sleep so they will not feel any pain or remember the operation. Your child's stomach must be empty before having a general anesthetic. They must follow eating and drinking guidelines to lessen the chance of throwing up, which could hurt their lungs.
If you do not follow the feeding guidelines, your child's operation will be cancelled.
If you are unsure of these instructions, call the clinic nurse or cleft lip and palate nurse coordinator a few days before the operation.
For more information about things such as what to pack and bring to the hospital, visit the Day before surgery page on the SickKids website.
On the day of the operation
Arrive at the hospital at least two hours before your child's operation so you can check in. You will be asked to fill in some forms with the nurse and your child will have a final assessment before the operation.
Pre-operative bathing with pre-packaged bathing wipes
To help prevent infection, your child will have a pre-operative bath using pre-packaged wipes. A nurse will explain this to you and your child. Watch this video to see the correct steps to perform a pre-operative bath using wipes.
During the operation
Your child will have a general anesthetic so that they will sleep through the operation. The anesthetic is given in the operating room by mask or through an intravenous (IV) line inserted into the back of your child's hand. The IV line is also used to give your child fluids and medication.
Constant observation room
After the operation your child will be moved to a constant observation room on the Plastic Surgery Unit. Your child will be closely monitored by a nurse.
Pain management after the operation
Your child will have pain after the operation. Pain medication will be given to help your child feel more comfortable, and to eat and drink with less pain. Your child's pain will generally be managed with medication that your child's surgeon will prescribe. Your child may be given pain medication on a set schedule or as needed. You know your child best. If you have concerns about your child's pain, speak to the health-care team.
Eating and drinking after the operation
After the operation your child will have an IV line in place for fluids until they are drinking well. Your child may not want to eat or drink after the operation. This may be because they are in pain. It will be important for your child to have pain medication about one hour before eating.
For about the first 24 hours after the operation, your child will only have clear fluids to drink. This will allow the sutures (stitches) to heal and help prevent infection. Some examples of clear fluids are water, low-acid apple juice and clear broth.
On the day after the operation, your child may have non-clear fluids (e.g., milk) in addition to clear fluids. Please encourage your child to drink a lot.
Solid foods
Before leaving the hospital, your child may be able to start eating pureed and soft foods. A soft diet includes foods such as pudding, yogurt, ice cream as well as well-cooked pasta, soft/scrambled eggs, soups, ripe bananas and ground/minced meats. A good guideline to follow is to allow your child foods that can be swallowed without biting. Your child will need to eat soft foods for 6 weeks following surgery.
It is important for your child to eat and drink to speed healing.
In order to protect the area of the operation and allow it to heal, please do not give your child anything hard or sticky to eat in the hospital and for 6 weeks after you return home. Your child should not eat hard/crunchy foods such as cookies, candies, hard/crunchy fruit, raw vegetables, french fries, bread crusts or toast, sandwiches or pizza. Your child should not eat sticky foods such as peanut butter, cheese spreads, and chocolate and hazelnut spreads.
Also, do not allow your child to use straws for 6 weeks following surgery.
If you have questions about what your child will be eating after the operation, please ask your child's health-care team.
Liquids or food coming out the nose
Food or liquids may come out of your child's nose when they are eating or drinking. Do not be alarmed. This is normal and may occur for several weeks after the operation until the incision line is completely healed.
Positioning your child: awake and asleep
The head of your child's bed will be raised slightly. This will help reduce the swelling that will occur around the area of the operation. It also helps to drain any blood and other fluids from your child's mouth. This drainage may continue up to 24 hours after the operation.
Your child may snore more than usual after the operation.
Activity
Your child may be up and out of bed soon after they return to the Plastic Surgery Unit.
Mouth care
It is important that you keep the area of the operation clean. It is normal for a small amount of blood to ooze along the suture line for up to 24 hours after the operation. Your child will rinse their mouth with either saltwater or mouthwash after they eat or drink anything. This includes liquid medications that your child receives. Your child's nurse will teach you how to do this.
Sore neck
Your child may have a sore neck after the operation. This is because of the way your child was positioned during the operation. This should go away after a few days. If it continues, please notify your surgeon.
Your child will stay in the hospital for 1 to 2 days
Your child will stay in the hospital for 1 to 2 days. Once your child has recovered from the operation and you feel able to take over their care, your child can go home. Before you go home, you will be given the instructions you need to care for your child and any follow-up appointment will be booked.
In general, one parent can stay overnight with their child during recovery.
Speech improvements
For some children, an improvement in hypernasality may be noticed shortly after surgery. However, other children may need more time and speech therapy, particularly if they continue to have incorrect speech patterns (compensatory articulation).
Your child will continue to be routinely monitored by a speech-language pathologist on the Cleft Lip and Palate Team to ensure they are achieving the best possible speech outcome and to answer your questions about speech.
Caring for your child at home after the operation
Once your child returns home, please follow these special instructions:
- To avoid damaging the area of the operation, give your child only soft food for a total of 6 weeks after the operation. Do not give your child foods that are hard or in big chunks. Do not use straws. After 6 weeks, your child can eat their usual foods.
- To keep your child's mouth clean, give them a drink of water after eating or drinking. Do this for 6 weeks after your child is home from the hospital.
- You can brush your child's teeth gently.
- Your child should not play sports for 2 weeks after the operation.
Follow-up with the surgeon and speech-language pathologist
Your child will have an appointment with the surgeon and speech-language pathologist 6 to 8 weeks after going home.
The surgeon will check your child's palate for healing.
The speech-language pathologist will assess your child's speech and determine if further speech therapy is needed. If needed, your child will be referred for speech therapy in your community.
Follow-up with the speech-language pathologist
Additional appointments will be made for 6 months after surgery and 1 year after surgery to:
- monitor the speech outcome of the surgery
- monitor for any changes in swallowing, sleeping or medical concerns
- continue to make recommendations
- answer your questions
When to seek medical attention
When at home, please follow the instructions in your discharge information to contact your child's health-care team right away if your child:
- is not eating or drinking
- has a fever
- has redness or oozing from the mouth
- has a foul smell from the mouth
- complains about a sore neck
At SickKids
Please download and use the Coming for Surgery Workbook to help inform and prepare you for surgery at SickKids. Everyone's journey is different, but this workbook provides information about preparing for surgery, the day of and after surgery as well as space for you to document information and questions you have. It also includes a packing list.