At the end of this chapter, you will be able to:
- Demonstrate how to assess your child’s respiratory status
- Identify signs of respiratory distress
Standard heart rate, respiratory rate and temperature ranges
When you are measuring your child's vital signs, you must always check the following.
- Heart rate
- Respiratory rate. To measure respiratory rate, count the number of times your child’s chest rises and falls in 60 seconds
- Temperature
- Oxygen saturation
- Blood pressure
The tables below from the Canadian Paediatric Society show the standard heart rate, respiratory rate and temperature ranges for children from birth to 18 years. Your health-care team will let you know the target heart rate and respiratory rate ranges for your child.
| Normal heart rate and respiratory rate ranges | ||
|---|---|---|
| Age | Heart rate (beats/min) | Respiratory rate (breaths/min) |
| Newborn | 93–182 | 26–65 |
| 1–3 months | 120–178 | 28–55 |
| 3–6 months | 107–197 | 22–52 |
| 6–12 months | 108–178 | 22–52 |
| 1–2 years | 90–152 | 20–50 |
| 2–3 years | 90–152 | 20–40 |
| 3–5 years | 74–138 | 20–30 |
| 5–7 years | 65–138 | 20–26 |
| 8–10 years | 62–130 | 14–26 |
| 11–13 years | 62–130 | 14–22 |
| 14–18 years | 62–120 | 12–22 |
| Temperature ranges | ||
|---|---|---|
| Method | Normal range (°C) | Fever (°C) |
| In the mouth (oral) | 35.5–37.5 | 38 or higher |
| In the anus or rectum | 36.6–38 | 38 or higher |
| Under the armpit (axillary) | 36.5–37.5 | 38 or higher |
| In the ear (tympanic) | 35.8–38 | 38 or higher |
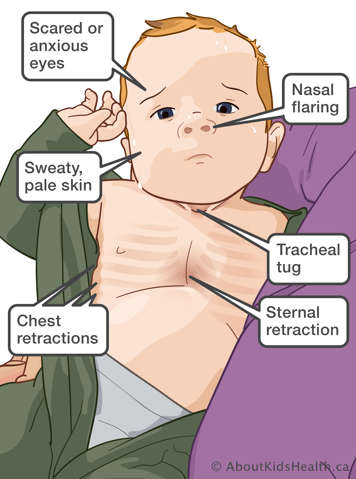
Signs of respiratory distress
When a child is experiencing respiratory distress (difficulty breathing), you may see one or more of the following signs.
Early signs of respiratory distress
- Increased effort to breathe.
- Using stomach muscles to breathe.
- Faster than normal breathing.
- Flaring of the nostrils – your child’s nostrils spread open when they breathe in.
- Head bobbing – head bobbing is caused by the use of neck muscles to assist in breathing. The child lifts the chin and extends the neck when breathing in and then allows the chin to fall forward when they breathe out.
- Abnormal breathing sounds such as wheezing or grunting. Wheezing is a whistling sound when your child breaths. Grunting is heard when your child breathes out as they are trying to get more air into their lungs.
- Sweating. You may notice sweat on your child’s head, but the skin feels cool, rather than hot. This may happen when your child’s breathing rate is fast.
Some children may experience respiratory distress along with a fever.
If your child's breathing is faster than usual, try to calm them down and see if their breathing rate returns to normal.
Later (more urgent) signs of respiratory distress
- Coarse crackling noises heard in your child’s chest or back when the child breathes. Some people refer to this as a "rattling" sound.
- Obvious distress or agitation.
- Retractions (pulling in of the skin of the neck, in between ribs or being pulled in at the bottom of the ribcage).
- Tripod position (sitting or standing while leaning forward and supporting the upper body with hands on the knees or on another surface).
- Cyanosis (pale or blue skin around the eyes, mouth, fingernails and toenails).
- Sleepiness or unresponsiveness.
If there is a "rattling" sound when your child breathes, encourage them to try to cough up the mucus to clear their lungs. Cyanosis indicates that your child is not getting enough oxygen. Unresponsiveness indicates that your child has a high level of carbon dioxide in their lungs.
Precaution
Call 911 or go to the nearest emergency department immediately if you see any late signs of respiratory distress in your child.
