By the end of this chapter, you will be able to:
- describe what manual pulmonary physiotherapy is and why it is used
- demonstrate how to perform manual pulmonary physiotherapy for your child with a tracheostomy tube
Manual pulmonary physiotherapy, or chest physiotherapy (CPT), can include a combination of manual techniques to loosen and remove secretions from the lungs. When secretions are thick, they can block air from moving into and out of your child’s lungs, making it harder to breathe. If secretions sit in the lungs for too long, they can cause a lung infection, making your child very sick. Pulmonary physiotherapy can help your child cough and remove secretions before they harm your child.
Your child’s health-care provider will prescribe the treatment most appropriate for your child.
How pulmonary physiotherapy clears the lungs
The trachea (windpipe) divides at the carina into smaller tubes called bronchi which themselves divide into smaller airways called bronchioles in the right and left lungs.

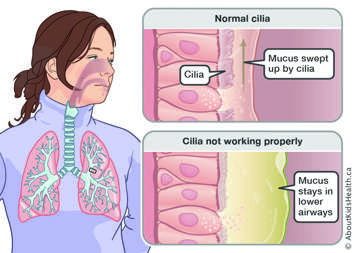
Cilia are hairs that are present on the lining of the lungs that sweep up the mucus to the upper and central airways so that secretions can be cleared and expelled.
When the cilia are not working properly, secretions stay in the lower airways.
Pulmonary physiotherapy techniques include manual therapy, such as percussion and expiratory vibrations that are done in modified postural drainage positions.
Types of pulmonary physiotherapy
Manual techniques
- Postural drainage, percussions, vibrations.
- Deep breathing and coughing.
Assisted coughing techniques
- Mechanical in-exsufflation (i.e., CoughAssist), lung volume recruitment (LVR), abdominal thrusts, lateral costal breathing, glossopharyngeal breathing.
Suctioning
- Using a suction machine to remove secretions from the nasal cavity (area behind the nose), mouth, throat, trachea and tracheostomy tube.
Benefits of pulmonary physiotherapy
- Clearance of secretions from the large and small airways.
- Includes manual techniques and the use equipment.
- Improve ventilation and gas exchange.
- Promote efficient breathing patterns.
- Improve quality of life.
When should I do pulmonary physiotherapy?
The best times for pulmonary physiotherapy are early morning and at bedtime. Early morning pulmonary physiotherapy helps remove secretions that have built up overnight. Bedtime pulmonary physiotherapy helps remove any remaining secretions so your child has a reduced need to cough and can sleep better through the night. Your health-care provider may want you to do pulmonary physiotherapy more often.
It is also best to do pulmonary physiotherapy before meals or at least one to two hours after eating. This will make it less likely that your child will feel sick or vomit.
Will my child need to use any medications?
Your child’s health-care provider may prescribe medications along with pulmonary physiotherapy to help open up your child’s airways and clear secretions from the lungs. These medications can be given with a puffer (called a metered dose inhaler or MDI) or a small nebulizer. Usually, you will give your child their medication before starting their pulmonary clearance routine.
How do I do pulmonary physiotherapy for my child?
Before you start
- Review the treatment plan outlined by the physiotherapist.
- Stop feeds (if appropriate) up to an hour prior to/during physiotherapy treatment.
- Provide prescribed medications before physiotherapy treatment to optimize treatment.
- Understand the risks and benefits of treatment.
- Apply oxygen saturation monitor.
- Take off rings and other jewelry on your hands or wrists.
- If your child’s clothing is tight or has thick seams, remove it.
- If your child is wearing clothing with buttons, remove it.
- Have your child wear a t-shirt or put a soft cloth over the area that you will percuss.
- Gather your supplies:
- a clock or a timer, to time how long you will percuss
- a percussor (if it has been prescribed)
- Position yourself and your child in a suitable place to do treatment, for example a bed, a couch or on a floor with pillows.
Performing pulmonary physiotherapy
Your physiotherapist will assess your child and create a treatment plan. The physiotherapist will teach you how to safely perform the physiotherapy techniques prescribed at home. However, there are some precautions and guidelines that are worth keeping in mind.
- Always percuss over the ribs. The lungs are protected by the ribs, so never percuss below the ribs or on the stomach, backbone, breastbone, nipples or on any lines/tubes or feeding tubes.
- One session of pulmonary physiotherapy should take 20 to 40 minutes. Usually, you will do manual pulmonary clearance in a number of prescribed positions and percuss all the areas. Your child's health-care provider or physiotherapist may have you percuss some areas more than others.
- Throughout the therapy session and immediately following therapy on your child, monitor your child’s:
- reaction to the therapy, including responses to pain
- discomfort
- shortness of breath
- heart rate and rhythm
- respiratory rate and pattern, including work of breathing
- cough and secretion production, including colour, quantity, consistency and smell
- breath sounds
- skin colour
- mental status (their emotions and awareness of their surroundings)
- oxygen saturation (as measured by a pulse oximeter)
- blood seen in the secretions
Postural drainage
Postural drainage involves changing your child’s position to help move secretions. The goal is to move secretions from the lower airways at the bottom of the lungs to the large airways in the middle. Using percussion and postural drainage together will help move secretions into the large airways so that they are easier to cough out.
- Lying or sitting in various positions so the part of the lung being drained is as high as possible.
- In children, modified postural drainage positions are used to decrease the risk of reflux/aspiration. This means, no head down positions are performed.
- Change in body position redistributes ventilation, thus optimizing oxygenation and blood flow.
Percussion
"Percuss" means to tap sharply. You can give your child percussions using a cupped hand, a percussing device or an electric percussor. Percussions:
- shake the chest and loosen secretions so they are easier to cough out
- move mucus into the larger airways
- are performed with a "Palm Cup" or using a tented hand, such that the hand is cupped with the palm facing downwards
- are done firmly with a steady beat making a hollow sound
- should not be painful
- should avoid the spine, breastbone, lower back and stomach
- should not be performed on bare skin – use a towel/blanket


If aerosol treatments have been prescribed, do them before percussion therapy, unless your child’s health-care provider tells you otherwise.
Expiratory vibrations
Expiratory vibrations are a technique that gently shakes the mucus while the child is breathing out, to move the mucus into the larger airways.

- A firm flattened hand is placed on the chest wall of the area that is being drained, and a shaking motion over the chest wall is performed in the direction of rib movement.
- Try to time vibrations with exhalation, although this can be challenging depending on the respiratory rate/depth of breathing.
Deep breathing and coughing
You can also encourage your child to breathe deeply and cough to loosen secretions and move them up into the large airways. Using deep breathing and coughing with clapping, percussion and postural drainage will help to bring up more secretions.
Precaution
If there is bright red blood in your child’s secretions, stop the pulmonary physiotherapy and call your health-care provider right away.
What should I expect during and after a manual physiotherapy session?
- Your child may cough more during or after manual physiotherapy. Coughing helps your child get rid of loosened secretions.
- Your child may cough for up to one to two hours after manual physiotherapy. Even if no secretions come up, this means the therapy is working.
- After swallowing a lot of secretions, your child may feel nauseous or throw up. As soon as your child is old enough to learn to spit, teach them how to spit secretions into a tissue. If your child does not stop throwing up, call your health-care provider.
If your child has been prescribed a CoughAssist machine, please refer to the page Mechanical in-exsufflation (CoughAssist) to learn more.
