If you have a child that needs to be mechanically ventilated, you will naturally have many questions and concerns.
What is mechanical ventilation?
The process of inhaling (breathing in) and exhaling (breathing out) is called ventilation. Mechanical ventilation involves using a ventilator (breathing machine) that can move air into your child’s lungs when they cannot breathe well enough on their own.
Your child may need continuous ventilation (24 hours a day) or ventilation for only for part of the day (for example at night). Your healthcare team will tell you what type of ventilation your child needs before they leave the hospital.
Why does my child need mechanical ventilation?
The body needs a constant supply of oxygen (in inhaled air) and a constant removal of carbon dioxide (in exhaled air), but certain lung, heart, neurological (brain and nervous system) or muscle diseases can make breathing more difficult.
Mechanical ventilators are used when the:
- brain cannot send signals to the lungs to breathe
- lungs are too stiff to expand fully
- lung tissue is damaged
- muscles for breathing are not strong enough to move air in and out of the lungs on their own
- heart is damaged, causing the lungs to work harder than usual.
Possible advantages of mechanical ventilation
With mechanical ventilation, your child may:
- have more energy
- have better concentration
- experience an increase in their appetite
- enjoy better quality sleep
- feel less fatigued
- experience fewer or less severe headaches.
Possible disadvantages of mechanical ventilation
Mechanical ventilation:
- may increase skin irritation from the tracheostomy tube
- may require you to carry more equipment and learn more skills
- can lead to increased costs for wheelchair adaptations and tracheostomy and ventilator supplies
- may increase your child's dependence on you or other caregivers
- can increase strain on caregivers.
Will my child need to rely on the ventilator completely?
A mechanical ventilator can offer total or partial support for your child’s breathing.
Total support is when the ventilator does all the breathing. Children who cannot breathe on their own need total support.
Partial support is when the ventilator assists with your child’s own breathing. A child who is able to breathe on their own but requires extra help between their own breaths needs partial support.
How long will my child need to use the ventilator?
Your child will have follow-up appointments at the long-term ventilation (LTV) outpatient clinic to review their ventilation needs. The LTV team will decide if and when your child is ready to begin weaning from the ventilator (gradually reducing ventilator use).
Weaning is usually done slowly, with careful observation and a lot of communication with your LTV team. Please note, however, that not every child will be able to have “ventilator-free time”.
What mechanical ventilation equipment do I need in my home for my child with a tracheostomy?
You will need various types of equipment to assist in your daily care tasks, including:
- two mechanical ventilators
- a manual resuscitation bag
- a portable suction machine
- humidification source
- inhaled medication
- portable oxygen
- an oximeter
- tracheostomy supplies
- emergency tracheostomy kit
- suction supplies
- stoma cleaning supplies.
Ventilators are provided in the province of Ontario by the Ventilator Equipment Pool (VEP). Your child’s healthcare team will give you more information about the VEP.
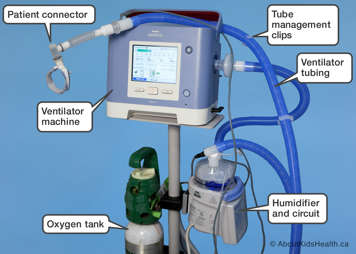
What types of ventilators are available for use at home?
Several types of ventilator are available, but, at present, the Philips Respironics Trilogy 200 ventilator is the machine that is provided through the Ontario Ventilator Equipment Pool program for those patients who qualify.
The Philips Respironics Trilogy 200 ventilator is licensed for use in children weighing at least 5 kilograms (11 pounds). This ventilator is intended for use in the home and can also be used as a portable ventilator.
Many detailed descriptions of a mechanical ventilator in this section will refer to the Trilogy 200 ventilator. If you are using a different ventilator, be sure to check the user instruction manual or ask your child's healthcare team for help.
| Your child’s ventilator: Make, model and prescription |
|---|
| Ventilator make (brand name): |
| Ventilator model: |