What is arthritis?
Arthritis means “joint inflammation”. Arthritides are a group of diseases that cause pain, swelling, stiffness and loss of motion in the joints. Arthritis in children is treatable. Most children with arthritis can expect to live normal lives with the help of health-care providers, rheumatologists, who are experts in childhood arthritis.
Juvenile idiopathic arthritis (JIA)
Juvenile idiopathic arthritis (JIA) is a type of chronic arthritis. There are several types of JIA, all of which involve long-term joint inflammation. Symptoms begin before children are 16 years old and the inflammation lasts for at least six weeks. The cause of JIA is unknown or "idiopathic". JIA may involve one or many joints and may cause other symptoms such as fevers or rash.
Systemic juvenile idiopathic arthritis (sJIA)
Systemic juvenile idiopathic arthritis (sJIA) is one type of JIA. Between 10% and 15% of all children with JIA have sJIA.
What is sJIA?
The immune system normally helps to fight off harmful, foreign substances such as bacteria or viruses by becoming more active. The immune system activity returns to normal when the body has successfully dealt with the harmful substance or infection. In an autoinflammatory disease, such as sJIA, the immune system becomes active for reasons that are not clear. It then remains active and begins to attack healthy cells and tissues. This results in inflammation of the joints causing them to become red, swollen, painful or hot to the touch and more widespread inflammation of the body resulting in features such as fever and rash.
Symptoms of sJIA
Children who have sJIA may experience prolonged, repeating fevers, which usually occur once or twice per day. When a fever is at its worst, a child may have a pink-coloured skin rash and may feel tired and achy or have widespread aches and pains.
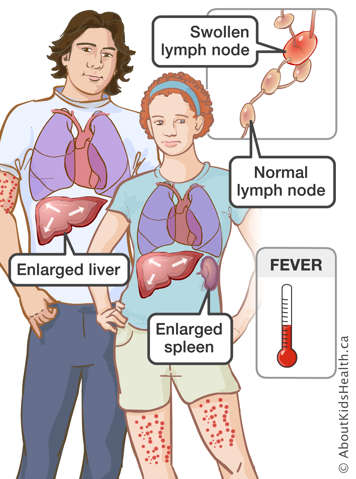
Inflammation or swelling of the internal organs such as the heart, liver, spleen and lymph nodes can also occur as a result of sJIA. It is common for children with sJIA to have anemia, where they do not have enough red blood cells and to have too many white blood cells. Arthritis may occur with the fevers or several weeks or months later.
Macrophage activation system (MAS) can also occur as a result of sJIA. In MAS, the immune system is uncontrolled and works in overdrive, leading to too much inflammation in the entire body.
Diagnosis of sJIA
Doctors may suspect a child has sJIA when there is ongoing joint pain or swelling, unexplained skin rashes and fever, swelling of lymph nodes or inflammation of internal organs. However, these problems can be caused by other diseases. Doctors will usually order blood tests, X-rays and sometimes additional tests to help diagnose the disease.
Treatment of sJIA
When first diagnosed, children with sJIA are often ill. Some may have to stay at the hospital while the disease and its symptoms are treated. Treatments control both the arthritis and other parts of the body affected by the disease.
The drugs most commonly used to treat sJIA are:
- Non-steroidal anti-inflammatory drugs, also called NSAIDs; these medicines are similar to acetylsalicylic acid (ASA) and ibuprofen
- Prednisone; this is a type of steroid
- Biologics (Anakinra, Tocilizumab)
There may be other treatments as well. Researchers are always learning more about sJIA and how to treat it.
Most drugs have some side effects. These are effects that are not part of the treatment. If your child is given any drug, the doctors or nurses will let you know about the drug's side effects and what that might mean for your child.
Living with sJIA
Your child’s daily activities
You and your child may need to make adjustments to your child’s usual activities. The pain and stiffness of their joints may make normal tasks harder to do. For example, sJIA may make it harder for your child to do things at school. Part of treatment for sJIA will be to try to lessen the effect of sJIA on your child's usual activities.
School and sJIA
Some children with more severe arthritis may not be able to take part in school activities. They may even have trouble writing. It may also be harder for them to get to school. They may have to miss school days because they are in the hospital or going to doctors' appointments.
Let the school know about your child's illness, they may be able to help. Your child's team can also contact the school to help with things like facilitating access to an elevator, transportation help with writing or an extra set of school books to use at home.
Your child's sJIA can affect the whole family
When a child has a disease, it can affect the whole family. The beginning of sJIA is often sudden and can be scary to both the child and the family. Sometimes the disease seems to get better, and at other times it suddenly seems to get worse. This can be hard on the whole family.
A child with sJIA, the parents or the child's brothers or sisters may sometimes feel guilty about what has happened. Other times, a brother or a sister may resent the extra attention a child with sJIA gets from their parents. If these things happen in your family, you can speak to a counsellor or a doctor. They may be able to help you through these hard times and may give you ideas to make things a little easier on everyone.
Try to keep your child with sJIA doing the same things that they did before the disease, whenever possible. If you are unsure of what your child can do, ask one of your health-care team members. Daily routines are important to children. Routines can include chores, school, visits with friends and play time. If routines change as little as possible, this will help your child feel better about how the disease has affected them. Social workers can give you advice on how to keep routines from changing too much. They can help you, your child and your family set realistic goals.
Follow-up care at the rheumatology clinic
Your child will be referred to a rheumatology clinic for follow-up care. Usually, a rheumatology clinic will have a team made up of doctors and nurses who have a lot of experience treating children with sJIA.
Other members of the rheumatology team may include:
- A physical therapist and an occupational therapist, who will help with your child's movement of joints and may teach your child different ways of doing things.
- A social worker and a child life specialist to help with emotional and behavioural problems that might result from the disease.
- A dietitian to help with your child's diet and nutrition.
Preparing for visits to the rheumatology clinic
Your child may need blood tests during a clinic visit. This will help doctors monitor the disease and check for possible side effects of the medicine your child may be taking. If your child needs to prepare for clinic visits in any other way, a member of the rheumatology team will let you know.
