The following guidelines will help you adjust insulin dosages at home. With practice and experience, this will soon become second nature. If you have any questions, or if adjusting the insulin dosage does not seem to help achieve target blood glucose (sugar) levels, contact your primary diabetes care team.
The sliding scale
MDI, TID, and BID regimens allow for insulin changes based on a sliding scale that adjusts the dose of rapid-acting insulin before meals and snacks based on blood sugar levels. The higher your child’s blood sugar level, the more rapid-acting insulin your child will have to take, as indicated by the sliding scale.
This method is more precise than using fixed rapid-insulin doses because it takes into account that blood sugar levels are not always in target range before a meal. However, this method is similar to fixed insulin doses because it assumes that your child will aim for a fixed amount of
carbohydrates per meal and snack.
Sliding scale values may differ between each meal because your child may be sensitive to insulin differently at different times of the day. The sliding scale can be used to adjust insulin doses in children using MDI, TID, or BID regimens.
Blood sugar targets
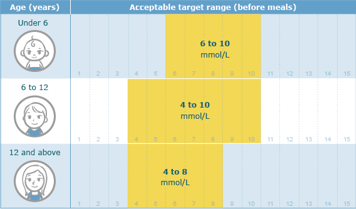
Blood sugar targets change as your child grows. Target ranges are set by your child’s ability (and your own) to understand diabetes, interpret signs and feelings of low blood sugar levels, and act on them.
Adjusting insulin when using a multiple daily injection routine (MDI)
You should adjust (increase or decrease) insulin dose by about 10% at a time. For example, you need to increase your child’s insulin dose because of high blood sugar readings. If your child’s usual insulin dose is 20 units, a 10% increase will equal to 2 units because (20 x 10)/100 = 2. You should then give your child 22 units of insulin because 20 + 2 = 22.
In case of high blood sugar levels
| Adjusting for high blood sugar levels on MDI | |
|---|---|
| If the blood sugar level is high for three days in a row before | Increase by 10% |
| breakfast | long-acting insulin (Lantus or Levemir) |
| lunch | pre-breakfast rapid-acting (Novorapid or Humalog) insulin |
| dinner | pre-lunch rapid-acting (Novorapid or Humalog) insulin |
| bedtime | pre-dinner rapid-acting (Novorapid or Humalog) insulin |
Increase insulin doses and call your diabetes team immediately if:
- Your child’s blood sugar level is high, and
- Your child is vomiting, and/or
- Your child has ketones in their urine, or your child is thirstier or urinates more than usual.
In this case, give an increased dose of insulin without waiting three days.
In case of low blood sugar levels
| Adjusting for low blood sugar levels on MDI | |
|---|---|
| If the blood sugar level is low for | Decrease by 10% the |
| 3 mornings in a week or
2 days in a row before breakfast | long-acting (Lantus or Levemir) insulin |
| 3 lunch time checks in a week or
2 days in a row before lunch | pre-breakfast rapid-acting (Rp or H) insulin |
| 3 dinner time checks in a week or
2 days in a row before dinner | pre-lunch rapid-acting (Rp or H) insulin |
| 3 bedtime checks in a week or
2 days in a row before bed | pre-dinner rapid-acting (Rp or H) insulin |
Further insulin doses adjustment tips
If your child follows an
insulin-to-carbohydrate (I:C) ratio and needs a dose adjustment as described in the above table, you must adjust the rapid acting insulin using the following (I:C) ratio guidelines.
If your child does not follow an I:C ratio, use the following rules as a guideline to adjust all other intermediate or long acting insulin dose:
- If the specific insulin dose is less than 15 units, adjust that insulin dose by 1 unit.
- If the specific insulin dose is between 15 units and 25 units, adjust that insulin dose by 2 units at a time.
- If the specific insulin dose is between 25 units and 35 units, adjust that insulin dose by 3 units at a time.
- If the specific insulin dose is more than 35 units, adjust that insulin dose by 4 units maximum at a time.
For example:
- A 10% increase on an I:C of 1:10 equals 1:11. With an I:C of now 1:11, your child would receive 1 unit of insulin for every 11 grams of carbohydrates eaten instead of 1 unit of insulin for every 10 grams of carbohydrates eaten. Overall, your child will receive less insulin.
- A 10% decrease on an I:C of 1:10 equals 1:9. In this case, your child would receive 1 unit of insulin for every 9 grams of carbohydrates eaten instead of 1 unit of insulin for every 10 grams of carbohydrates eaten. Overall, your child will receive more insulin.
See the section
Adjusting insulin when using an insulin pump for further details.