Your child is going home with a nephrostomy tube. The tube needs care at home. A nurse will teach you how to care for the tube before your child leaves the hospital.
What is a nephrostomy tube?
A nephrostomy tube is a small flexible tube placed through the lower back that drains urine from your child's kidney to the outside of your child's body. It is also called a nephrostomy catheter. A nephrostomy tube is inserted when there is an obstruction (blockage) to the normal flow of urine.
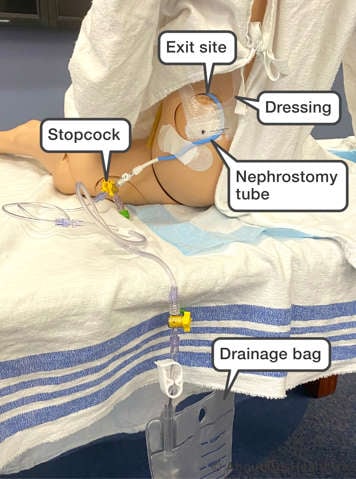
The place where the tube comes out of your child's body is called the exit site. When your child leaves the hospital, the exit site will be covered with a clear dressing. The tube will connect to a drainage bag. The flow of urine will be controlled by a valve called a stopcock that can be switched on and off.
Care of the nephrostomy tube
Your child's nurse will show you how to care for the tube before your child goes home from hospital.
To care for your child's nephrostomy tube, follow these instructions:
- Wash your hands well with soap and water before and after you touch the tube or drainage bag.
- Check the tube every hour for leaks, loops or kinks. Loops and kinks will block the flow of urine. You should check the tube before your child goes to bed and as soon as they get up. If your child is a restless sleeper, you may also wish to check the tube at least once overnight.
- The tube should be well-secured to your child’s body to prevent tube movement at the insertion site and accidental tube removal. You can attach the tube to their body with medical tape or a designated securement device such as Grip-Lok.
- Make sure that the dressing is dry and attached to your child’s body. It is okay for your child to take a shower while the tube is in, but make sure that the tube is taped to their body so that it does not get pulled out. You will also need to change the dressing if it becomes wet or loose after a shower.
- If a stitch (suture) is present at the exit site, check that it is still in place.
- Always keep the catheter drainage bag lower than your child's kidney, as this will prevent the urine from flowing back into kidney. This includes when your child is standing, sitting, or lying down.
- Check the amount of urine that is draining and empty the drainage bag regularly. It is recommended the bag be emptied when it is half full to prevent the urine flowing back into the kidney.
- It is okay to use the same drainage bag for up to two weeks. Replace the bag if it gets stiff, discoloured with sediment, or if it leaks.
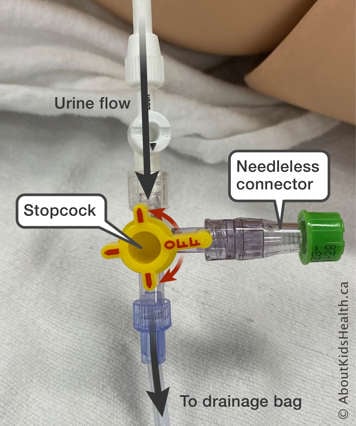
- To change the drainage bag, turn the stopcock so that the “OFF” arm points towards your child, then disconnect the drainage bag. Clean the connection area and new drainage bag with an alcohol swab before putting them back together.
Changing the dressing
Home care nurses usually change the dressings on a nephrostomy tube, but if you have been taught how to do it and you are comfortable, you can change the dressing yourself.
To keep the exit site healthy, you should change the dressing every seven days, or every time you notice the dressing is wet. If your child is being treated for a visible or suspected infection at the exit site, you should change your child’s dressing daily.
Always change the dressing if:
- Drainage or bleeding is present at the exit site
- The dressing is soiled or loose
Supplies for changing your child’s dressing include:
- Wound cleaning solution: Chlorhexidine (or povidone iodine, if your child is allergic to chlorhexidine)
- This is available as a packaged swab/applicator
- Two pairs of clean gloves
- A new clean dressing
To change the dressing, follow these steps:
- Wash your hands with soap and water.
- Put on a pair of clean gloves.
- Gently remove the old dressing, making sure there is no signs of infection or bleeding at the site. Leave the medical tape or securement device in place.
- Remove the gloves and wash your hands with soap and water again.
- Open the package of the new dressing and leave the dressing on the package or any other clean surface. Try not to touch the dressing afterwards.
- Put on the second pair of clean gloves.
- Use the swab/applicator to clean around the tube with the wound cleaning solution for 30 seconds. Allow the site 2 minutes to dry.
- Apply the new dressing to the exit site.
- Remove the gloves and wash your hands using soap and water.
After changing the dressing, always check that the nephrostomy tube is draining well. It is also important to check your child’s skin daily for signs of infection at the entrance site.
Flushing the nephrostomy tube with normal saline
If the flow of urine from the tube decreases or stops, the tube may need to be flushed with a solution called normal saline. This clears any small pieces of waste that might be blocking the catheter from draining. Flushing is also described as 'instilling'.
Supplies:
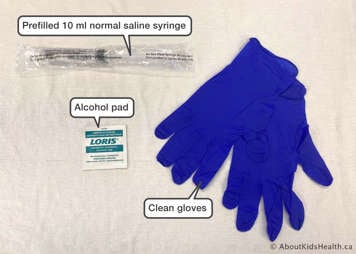
- Prefilled 10 ml normal saline syringe
- Alcohol pads
- Clean gloves
To flush the tube, follow these steps:
Wash your hands with soap and water and put on a pair of clean gloves.
-

Using friction, scrub the needleless connector on the stopcock closest to your child’s body using an alcohol pad for 15-30 seconds. Allow the stopcock to dry completely for approximately 15 seconds.
-

Turn the position of the stopcock so that the “OFF” arm points towards your child. Attach a syringe of normal saline to the needleless connector and slowly push the plunger towards the bag, flushing with 5 ml of normal saline.
-

Turn the position of the stopcock so that the “OFF” arm points towards the bag and slowly push the plunger to flush the remaining 5 ml of normal saline towards your child.
-

Turn the position of the stopcock so that the “OFF” arm points towards the now empty syringe. Remove and discard syringe.
Remove the gloves and wash your hands with soap and water.
If you meet resistance
If you meet a high amount of resistance while you are pushing the plunger and the normal saline solution does not flow, follow these steps:
- Check the tubing for kinks and try again.
- Make sure that you turn the position of the proximal stopcock so that the “OFF” arm points towards the syringe, so the nephrostomy tube is open.
- If there is still resistance and urine does not flow, call your child's doctor or nurse.
Do not pull the saline out of the tube with the syringe
Flushing a nephrostomy tube is not the same as irrigating it. Irrigation is putting a large amount of normal saline into the tube leading to the kidney and then pulling it out with a syringe. Never do this yourself. Irrigation should only be done by a doctor or a nurse.
Problems that require medical attention
There can be problems with the nephrostomy tube that you should not try to solve by yourself. Call your child's nurse or go to the hospital if any of the following things happen:
- The tube comes out. Do not try to put the tube back in yourself.
- There is a change in urine colour. It is normal for the urine to be a little pink from small amounts of blood one day after the procedure. If there is a further reddening of urine colour, call your child's nurse or doctor.
- Less urine comes out of the tube. Normally, you should see a slow, continuous flow of urine. If less than the regular amount of urine is coming out of the tube, flush the tube and then call your child’s nurse or doctor.
- Your child develops a fever of 38.5 °C or chills. This could be a sign of infection.
- Your child has pain in the stomach or back.
- Your child is unwell, vomiting or has nausea.
Accidental removal of the nephrostomy tube
If the nephrotomy tube is accidentally removed, you should do the following:
- With gloved hands (either sterile or clean, whichever is readily available) block the exit site.
- Call for assistance to place a clean dressing at the exit site.
- Inform your child’s doctor or nurse as soon as possible and they will instruct you on bringing your child back to the hospital.
At SickKids
If you have concerns and it is after working hours, see your primary care provider or go to the nearest Emergency Department. You can also call the Hospital for Sick Children switchboard at (416) 813-7500 and ask them to page a member of your child’s health-care team.