What is optic neuritis?
Optic neuritis occurs when there is swelling and inflammation of the optic nerve of the eye.
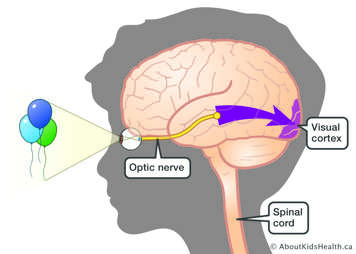
The optic nerve carries visual information from your eye to the visual cortex in the brain about what you are seeing. The two optic nerves along with the brain and spinal cord make up the body’s central nervous system (CNS). The CNS is referred to as “central” because it combines information from the whole body and coordinates activity. When the optic nerve becomes inflamed, it cannot protect the optic nerve fibres as effectively, which can affect how visual information is sent to the brain.
How does inflammation affect the optic nerve?
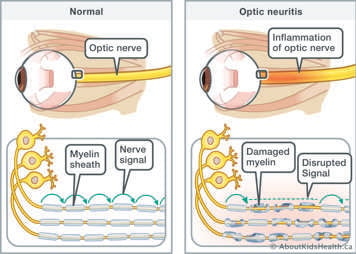
The optic nerve is made up of millions of nerve fibres. These fibres relay messages about what you are seeing to your brain, which creates visual images. The optic nerve has a fatty protective covering called “myelin” that insulates and protects the nerve fibres.
The body’s immune system sometimes creates inflammation against its own tissues. When this happens, the immune cells can mistakenly attack the myelin of the optic nerve, which causes the myelin to swell and break down. If the myelin is swollen and damaged, the optic nerve cannot effectively send visual information to the brain. This causes blurry or reduced vision and other symptoms, such as eye pain and headaches, due to the swelling and pressure.
What are the signs and symptoms of optic neuritis?
In children, optic neuritis usually occurs in both eyes (bilateral), but it may also occur in just one eye (unilateral).
Most commonly, your child will have a sudden decrease or loss of vision over a few days or weeks.
Other symptoms can include:
- changes in colour perception
- changes in brightness
- loss of portions of peripheral or central vision
- total vision loss (rare)
What can cause optic neuritis?
The exact cause of optic neuritis is not known. Sometimes, optic neuritis can occur after your child has had a viral infection. The immune system can be triggered by a virus to mistakenly attack your own body’s tissues, such as the myelin sheath (covering) of the optic nerve. This process is called an autoinflammatory or autoimmune process.
Optic neuritis can also occur with chronic illnesses, such as in multiple sclerosis (MS), or be a symptom of another demyelinating disorder, such as acute disseminated encephalomyelitis (ADEM) or neuromyelitis optica spectrum disorders. Sometimes, no specific cause is identified.
How common is it?
Optic neuritis is more common among the Caucasian population and those living in high geographic latitudes (far from the equator). It is more common among females than males. It can occur at any age.
How long do optic neuritis symptoms last?
Decreased vision or “scotoma” (dark spot in the vision) can last for several weeks to months. The visual symptoms will typically improve gradually. For many children, vision returns to normal or near normal.
What tests can be done to diagnose optic neuritis?
Your child may have the following tests to be diagnosed with optic neuritis:
- dilated eye exams to look for swelling of the optic nerve head (disk)
- neurological exams
- lumbar puncture to check the cerebral spinal fluid for proteins and cells associated with inflammation
- MRI
- visual evoked potentials (VEPs) to check optic nerve function
- blood work, including testing for viruses and antibodies that may trigger the immune system in the body
What are the treatments available for children with optic neuritis?
Medications are the treatment of choice for children with optic neuritis to reduce inflammation of the optic nerve and speed recovery.
The first line of therapy is corticosteroids, called methylprednisolone, through an intravenous (IV) once per day for three to five days. Your child will need to stay in hospital to receive this medication. Afterwards, if needed, your child may be given an oral steroid medication called prednisone.
What are some side effects of steroids to watch for?
Steroids are usually well tolerated by children. Some side effects can include:
- difficulty sleeping (insomnia)
- weight gain
- suppressed immune system
- moodiness or behavioural changes
- increase in blood pressure
- increase in blood sugar
Steroids can also irritate the stomach lining. Your child will be given a medication to protect their stomach lining while on steroids.
Methylprednisolone can often treat optic neuritis well on its own. In some cases, children may require another anti-inflammatory treatment called plasmapheresis or plasma exchange (PLEX).
Children with optic neuritis have a good chance of nearly complete to complete recovery of vision. Recovery usually starts within days of treatment and may continue up to one year.
Possible complications of optic neuritis
One possible complication of optic neuritis is reduced vision in the affected eye due to scarring. Often, when treated quickly with anti-inflammatory therapies such as corticosteroids, the vision will return to normal or near normal. In some cases, children can have recurrence of optic neuritis in the same eye or in the other eye. If this happens, the optic neuritis is again treated with corticosteroids and your child may be started on another medication to prevent the optic neuritis from recurring in the future.
How to help your child with reduced vision due to optic neuritis
Your child may have difficulty reading at a distance or completing their schoolwork due to the reduced vision. Your child could be moved closer to the white/chalk board in their classroom and given large print reading. Changing the font to a larger size on computers and devices can also be helpful as well as providing bright working environments at home and at school.
Follow-up care
Follow-up will be scheduled with your neurologist or nurse practitioner and ophthalmologist in clinic.
Your child will require follow-up MRIs, assessments in Neurology and Ophthalmology clinics and visual testing to assess for response to treatment and recovery.
Follow-up appointments and tests will be discussed upon discharge from hospital.
Will my child be at risk for developing recurrent optic neuritis?
Many children will experience optic neuritis as a one-time event. Your child’s health-care team will continue to monitor them for many years for recurrence of optic neuritis. Some children experience a recurrence of optic neuritis and may require immune-suppressant medications to prevent recurrence. Children who are positive for autoantibodies such as anti-NMO and anti-Mog may be at risk for recurrence of optic neuritis. You can read more about antibody-mediated inflammatory disorders.
When to seek medical attention
If your child develops blurry vision, eye pain or other symptoms of optic neuritis or other neurologic symptoms once they are at home, please contact your Neurology Team as soon as possible or bring your child to the Emergency Department.
Who will be involved in my care at SickKids?
Your child will be seen by:
- an eye doctor (ophthalmologist)
- a neurologist
- a nurse practitioner
- nurses
References
Benseler, S., Sickand M., Twilt, M. (2013, May 13). Inflammation and the immune system. AboutKidsHealth. Retrieved from http://www.aboutkidshealth.ca/En/HealthAZ/ConditionsandDiseases/InflammatoryConditions/Pages/Inflammation-and-the-immune-system.aspx
Optic neuritis. (2016, March). American Association for Pediatric Ophthalmology and Strabismus. Retrieved from https://www.aapos.org/terms/conditions/84
Optic neuritis. (2016). Mount Sinai Hospital. Retrieved from http://www.mountsinai.org/patient-care/health-library/diseases-and-conditions/optic-neuritis
Optic neuritis in children. (n.d.). Boston Children’s Hospital. Retrieved from http://www.childrenshospital.org/conditions-and-treatments/conditions/o/optic-neuritis-on/overview
Perez-Cambrodi, R.J., Cubillana, A.G-H., Merino-Suarex, M.L., Pinero-Llorens, D.P., Lana-Ochaita, C. (2014). Optic neuritis in pediatric population: A review in current tendencies of diagnosis and management. Journal of Optometry, 7, 125-30. DOI: 10.1016/j.optom.2013.12.008
Schatz, M.P. (2015, November 30). Childhood optic neuritis. Retrieved from http://emedicine.medscape.com/article/1217290-overview