What is pancreatitis?
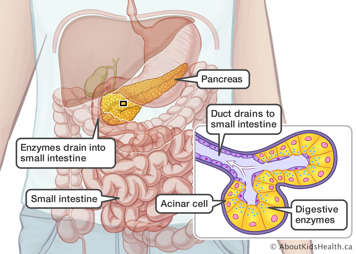
Pancreatitis is an inflammation of the pancreas. The pancreas is an organ that is part of the gastrointestinal system and is located just behind the stomach. This organ produces insulin and glucagon which are hormones that regulate blood sugar levels in the body. But the pancreas also plays a major role in digestion. It produces the necessary enzymes that help digest the food we eat.
There are two types of pancreatitis: acute and chronic.
- Acute pancreatitis means the condition arises suddenly and usually gets better after a short period of time.
- Chronic pancreatitis means that the condition develops gradually and keeps coming back. Chronic pancreatitis is rare in children and is usually part of an inherited condition.
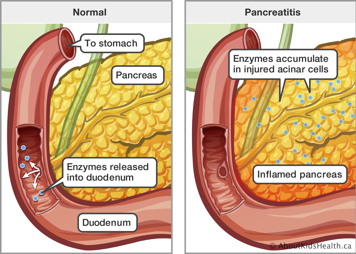
Specialized cells in the pancreas called acinar cells produce digestive enzymes. These enzymes are normally released into the small intestine. In pancreatitis, an event causes an injury to the acinar cells, which triggers an inflammatory reaction. This inflammation can be strong enough to damage the pancreas.
Signs and symptoms
Acute pancreatitis
Some signs and symptoms of pancreatitis are:
- intense stomach pain (abdominal pain), which is usually in the upper abdomen, just below the sternum (breastbone). The pain may also be felt in the back.
- nausea and vomiting, which becomes worse after eating
- fever
- loss of appetite
Your child may be more comfortable lying on their side because moving increases the pain. Your child may also feel very ill, restless and uncomfortable.
Less common symptoms include:
- ileus (where the intestines stop contracting and may become blocked)
- swollen belly (abdomen)
- jaundice (condition causing the skin, body tissues and fluids to have a yellowed colour)
- fluid build-up in the abdomen
- build-up of fluid around the lungs that can make breathing difficult
In babies and toddlers, symptoms can be more difficult to recognize. They include:
- irritability
- swollen abdomen
- fever
- bellyache (abdominal pain)
- loss of appetite
Chronic pancreatitis
Chronic pancreatitis is also an inflammation of the pancreas. Instead of the inflammation getting better as in acute pancreatitis, the inflammation continues in some more susceptible children and causes permanent damage to the pancreas. Genetic and environmental factors may be responsible for one's susceptibility to pancreatitis. Children usually experience signs and symptoms identical to those caused by acute pancreatitis, such as intense abdominal pain that worsens after eating a meal, nausea and vomiting and episodes will be recurrent.
The condition lasts for long periods of time and slowly destroys the functions of the pancreas. For example, the pancreas may lose its ability to produce insulin. As a result, children can develop glucose intolerance. Chronic pancreatitis can also cause weight loss because of poor digestion. Diagnosing chronic pancreatitis relies on changes in diagnostic imaging and blood work in addition to clinical symptoms.
Causes of pancreatitis
Pancreatitis can be due to other conditions
A number of conditions may trigger pancreatitis; some of these are associated with other conditions.
- Biliary disease. Ten per cent to 30% of children with pancreatitis may suffer from gallstones. Treating the condition may help restore normal pancreatic function.
- Multisystem diseases. Twenty per cent of cases of acute pancreatitis may be due to conditions affecting several organs or organ systems, such as sepsis, hemolytic-uremic syndrome or systemic lupus erythematous.
- Metabolic diseases. Metabolic disorders may be responsible for 2% to 7% of acute pancreatitis cases. Examples include errors of metabolism children are born with high lipid levels or high calcium levels.
- Infections. Acute pancreatitis is sometimes diagnosed when a child suffers from an infection. However, it is difficult to establish a direct relationship between the two conditions. Some of the infectious diseases that have been linked to pancreatitis include: mumps, rubella, CMV, HIV, adenovirus and coxsackie virus B.
- Anatomic abnormalities. Abnormalities in the structure of the pancreas or biliary tract can lead to pancreatitis.
Pancreatitis can be due to medication
Medications are thought to cause one quarter of the cases of pancreatitis. The most common medications that are thought to cause pancreatitis are valproic acid, L-asparaginase, prednisone and 6-mercaptopurine. It is not fully understood why these medications may cause pancreatitis. One reason may be because children treated with these drugs have other conditions that may predispose them to pancreatitis.
Pancreatitis can be due to trauma
Another possible cause of pancreatitis is trauma. An injury to the pancreas may provoke acute pancreatitis. This type of injury may happen in a car crash, sports, falls or child abuse.
Other causes
Pancreatitis may be hereditary, which means it was passed on by one or both parents. It can be associated with hereditary conditions such as cystic fibrosis. It can also be caused by a genetic mutation that is found in the child but not in the parents.
Finally, there are a large number of cases of pancreatitis where the cause is unknown. This is called idiopathic pancreatitis.
Diagnosis
The doctor who examines your child will use the signs and symptoms in addition to lab and imaging tests to diagnose your child.
To determine if the pancreas is working properly, a blood test can measure the levels of the digestive enzymes amylase and lipase. If the levels of these enzymes are high then there is probably something is wrong with the pancreas.
Your child will probably have an ultrasound, CT scan (computed tomography scan) or MRCP (magnetic resonance cholangiopancreatography). An ultrasound can help rule out other possible causes of stomach pains, such as appendicitis or gallstones. It also shows if the pancreas has changed in position or size because of swelling.
Treatment
Treatment of acute pancreatitis
Your child may need to stay in the hospital for monitoring and to receive appropriate care and fluids for hydration. Usually, children get better in two to four days.
There are no specific medications to treat pancreatitis. The initial part of treatment is pancreatic rest. This means your child will eat nothing by mouth. Your child will likely have an intravenous (IV) line inserted in the vein of an arm or leg. Your child will get fluids, anti-nausea medicines and pain medication.
Treatment of chronic pancreatitis
Children with chronic pancreatitis may have episodes of acute pancreatitis that would be treated as described above. Management of chronic pancreatitis requires a long term-plan.
Your child's doctor will try and identify the cause of the condition. They will help manage the pain. They will monitor pancreatic functions over the long-term to make sure they detect any pancreas-related digestive problem and diabetes as early as possible.
Your child may be given antibiotics in case of infection. Also, it is recommended to avoid alcohol and smoking because it may worsen the condition. Your child's doctor will talk to you about what other treatment options are best for your child's situation.
Complications
Complications of acute pancreatitis are uncommon in children. The most common complication is a collection of fluid that forms around the pancreas. This is called a pseudocyst. A pseudocyst can become infected, bleed or rupture. The fluid may go away on its own with time. However, if the fluid collection is large or if it is causing symptoms, then your doctor might suggest draining the fluid to avoid further complications.
When to see a doctor
See a doctor if your child has the following symptoms:
- severe pain in the upper part of the belly
- nausea and vomiting
- loss of appetite
- jaundice
Your child may show physical changes when their condition is serious or when their condition gets worse. Parents and caregivers can learn how to spot these signs in order to seek help from a health-care provider.