During a blood and marrow transplant (BMT), doctors replace your child’s bone marrow system with healthy blood stem cells. These stem cells are young, immature cells that grow into more specialized cells. The stem cells your child receives during the transplant will grow into mature blood cells. During the transplant, your child’s bone marrow absorbs the healthy stem cells. Once inside the bone marrow, the cells start to produce healthy blood cells. This process is called engraftment.
Your child may need a BMT because:
- they have too few blood stem cells
- their blood cells do not work properly
- it is part of their cancer treatment
There are two types of transplants:
- Allogeneic stem cell transplant. In this type of transplant, your child receives stem cells from a donor. In many cases, the donor is often a related family member, such as a sibling.
- Autologous stem cell transplant. In this transplant, your child donates their own blood stem cells.
Where do blood stem cells come from?
Healthy blood stem cells can come from three different parts of our body.
Bone marrow
The spongy tissue inside our bones is called bone marrow. We have blood stem cells inside the marrow of our breast bone, skull, hips, ribs, and spine. Our bone marrow contains the largest amount of blood stem cells inside our body. There is about one stem cell in every 100,000 blood cells inside our marrow.
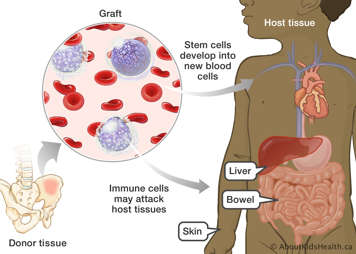
During a transplant, some immune cells from the donor get transplanted as well. Normally, immune cells trigger an immune response by attacking cells that do not belong there, such as viruses or bacteria. After the transplant, the immune cells need to adjust to their new environment (your child’s body). Sometimes these immune cells are unable to recognize the organs and tissues inside your child’s body. If this happens, they start to attack and damage your child’s cells. This is an immune complication called graft vs host disease (GVHD).
Research shows that patients who receive stem cells from the marrow are less likely to develop GVHD. This is why bone marrow transplants have historically been the most common source of blood cells.
For more information, please see the page on Graft-versus-Host Disease in the While Your Child Is in the Hospital section.
To collect blood stem cells directly from the marrow, doctors inject a needle into the top of the hip bone, called the posterior superior iliac crest.
Circulating (peripheral) blood
Doctors can also collect donor blood stem cells indirectly from the blood that circulates in our body. This is called a peripheral blood stem cell transplant. In this transplant, the donor takes a synthetic protein called G-CSF. The protein moves the blood stem cells from the marrow into the blood stream.
In addition to stem cells, peripheral blood also contains a type of white blood cell which helps fight infection, called T-cells. If the donor has a significant HLA mismatch, we need to process the peripheral blood to take out unwanted T-cells, so the final product just contains stem cells. Lab specialists do this using a technique called CD34+ selection. Stem cells have a special protein on their surface called CD34+. The lab technicians filter the peripheral blood sample through a machine which separates cells. This machine selects cells with CD34+ on their surface (and hence selects for stem cells). Once purified, the stem cells are stored and ready for transplantation.
Cord blood
Doctors can also collect blood stem cells from the umbilical cord, which connects a baby to the placenta. They are collected from the umbilical cord and placenta after the baby is born. This is different from embryonic stem cells, which are collected from an early fetus.
Cord blood stem cell transplants are a relatively new procedure. The first transplant was performed in 1988. Cord blood does not contain as many blood stem cells as peripheral blood or bone marrow. This is why they are generally used for younger children who may not need as many stem cells as teenagers.
Choosing the source of stem cells
Your child’s doctor may take stem cells from peripheral blood rather than bone marrow, for the following reasons:
- If the donor is smaller in size than your child. Generally, this is true if the donor is less than half the size of the patient. After taking GCS-F, more stem cells can be taken from the peripheral blood than taking it directly from the bone marrow. This avoids taking a larger volume of blood from the donor.
- If a parent is a donor, which is uncommon. In this case, at least half of the HLA proteins on the parent’s blood cells are identical to the child’s cells. This is called haploid-identical allogenic transplant. Peripheral blood is used because we can process the stem cells via CD34+ selection. This will get rid of unwanted cells in the sample. Bone marrow is too thick to process.
- If your child is having a transplant and is being treated for a malignant disease (such as leukemia). Sometimes, the T-cells in the donor’s blood may trigger an immune response against the diseased cells in the patient. When the donor’s T-cells kill the patient’s malignant cells, this is called the graft vs leukemia effect (GVL). Research shows that using peripheral blood to induce GVL can lower the likelihood of relapse occurring.
How common is BMT?
Currently in Canada, there are about 1200 BMT every year, 170 of which are done in children. As procedures and ability to find matching donors improve, transplants are becoming a better treatment option for more people. For example, researchers are studying BMT as part of a treatment option for a type of brain tumour called medulloblastoma. Treating medulloblastomas usually involves high-dose chemotherapy, which can also destroy healthy immune cells. This places children at risk of infection. Researchers are currently testing whether adding BMT to the treatment plan can help children receive chemotherapy without putting too much strain on their immune system. To do this, doctors infuse the child with new blood stem cells between intervals of high-dose chemotherapy. This gives their marrow time to recover from the chemotherapy.