What are vascular malformations?
Vascular malformations are abnormal clusters of blood vessels that develop before birth. Some may not be noticed until many years later. Some vascular malformations cause no problems, but others interfere with blood flow and can be dangerous. Vascular malformations can cause disfigurement, pain, troublesome swelling, bleeding and infection. Some are associated with growth abnormalities in the affected body part. Vascular malformations can be treated with minimally invasive procedures such as embolization, laser and sclerotherapy. The type of treatment your child will receive will depend on the location, size and type of vascular malformation.
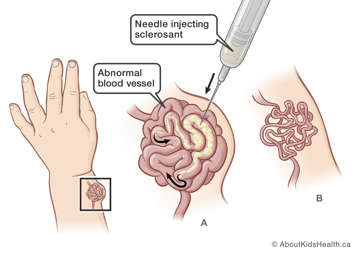
What is sclerotherapy?
Sclerotherapy is sometimes called “sclero”. A needle is inserted into the skin and injects a solution (sclerosant) into the abnormal blood vessel. This makes the blood vessel shrink. Sometimes the malformations can enlarge again and sclerotherapy may be done in stages.
Sclerotherapy is done using image guidance by an interventional radiologist. Most often, sclerotherapy is done alone or in combination with laser or embolization.
Risks of sclerotherapy for your child
Sclerotherapy is considered a low-risk procedure. The risk may increase depending on your child’s condition, age and health.
The risks of sclerotherapy can include:
- swelling (to be expected)
- pain
- skin blisters, ulcers, scars or skin staining
- nerve damage
- kidney damage
- interruption of blood supply to the treated area
- heart and lung complications
- loss of arm or leg (very rare)
Visiting the clinic before the procedure
Your child will need to have a clinic visit with the interventional radiologist before the procedure to decide on the best treatment options.
During the visit, your child may:
- see physiotherapy and/or occupational therapy
- obtain information about pressure garments
- have a health assessment to make sure they are healthy and it is safe to have sedation or general anaesthesia
- be sent for photography
- review the consent forms
- have blood work done, if needed
Giving consent before the procedure
Before the procedure, the interventional radiologist will go over how and why the procedure is done, as well as the potential benefits and risks. They will also discuss what will be done to reduce these risks and will help you weigh any benefits against the risks. It is important that you understand all these potential risks and benefits of sclerotherapy and that all of your questions are answered. If you agree to the procedure, you can give consent for treatment by signing the consent form. A parent or legal guardian must sign the consent form for young children. The procedure will not be done unless you give your consent.
How to prepare your child for the procedure
Before any treatment, it is important to talk to your child about what will happen. When talking to your child, use words they can understand. Let your child know that medicines will be given to make them feel comfortable during the procedure.
Children feel less anxious and scared when they know what to expect. Children also feel less worried when they see their parents are calm and supportive.
If your child becomes ill within two days before the procedure
It is important that your child is healthy on the day of their procedure. If your child starts to feel unwell or has a fever within two days before sclerotherapy, let their health-care provider know. Your child may need to be rescheduled.
Food, drink, and medicines before the procedure
- Your child’s stomach must be empty before sedation or general anaesthetic.
- If your child has special needs during fasting, talk to their health-care provider to make a plan.
- Your child can take their regular morning medicine with a sip of water two hours before the procedure.
- Medicines such as acetylsalicylic acid (ASA), naproxen or ibuprofen, warfarin or enoxaparin may increase the risk of bleeding. Do not give these to your child before the procedure unless they have been cleared first by their health-care provider and the interventional radiologist.
On the day of the procedure
Arrive at the hospital two hours before the planned time of your child’s procedure. Once you are checked in, your child will be dressed in a hospital gown, weighed and assessed by a nurse. You will also be able to speak to the interventional radiologist who will be doing the sclerotherapy and the anaesthetist who will be giving your child medication to make them comfortable for the procedure.
During sclerotherapy, you will be asked to wait in the surgical waiting area.
Your child will have medicine for pain
It is important that your child is as comfortable as possible for the procedure. They may be given local anaesthesia, sedation or general anaesthesia. The type of medicine that your child will have for the procedure will depend on your child’s condition and the treatment option the interventional radiologist uses for sclerotherapy. Most children receive general anaesthetic for sclerotherapy.
How sclerotherapy is done
The interventional radiologist inserts a needle through your child's skin into the abnormal blood vessel and injects a dye called contrast. The dye is a clear, colourless liquid that helps to outline the blood vessel so it will show up on an X-ray (fluoroscopy). The interventional radiologist can use fluoroscopy as a guide for the sclerotherapy injection. Ultrasound is often used in combination with fluoroscopy before the injection of the sclerosant to identify the abnormal blood vessels.
Next, the interventional radiologist injects a the sclerosant directly into the abnormal blood vessel. Sclerosant causes clotting and shrinking of the blood vessel. The interventional radiologist gives injections of the sclerosant into different areas of the vascular malformation if needed.
Each treatment will take about one to two hours, and sometimes longer, depending on the complexity of the malformation.
After sclerotherapy
Once sclerotherapy is complete, your child will be moved to the recovery area. The interventional radiologist will come and talk to you about the details of the procedure. As soon as your child starts to wake up, a nurse will come get you.
In the recovery area, your child will receive fluids through an intravenous (IV) tube. Your child should drink plenty of fluids when they wake up.
If a foley catheter has been placed to monitor your child’s urine output, it will remain in for four hours and will be removed before your child goes home.
It is important that your child passes urine at least once before going home.
Going home
After sclerotherapy, most children go home the same day. Your child will be ready to go home when they are wide awake, have started to eat and drink, and are making urine. Usually, this happens four hours after the procedure.
The areas that were injected are normally swollen for one week and bruised for two to three weeks following the procedure. The skin close to the abnormal blood vessel may blister or be sore.
Your child may have some discomfort after the procedure which may last one to two days.
At home, you can give your child acetaminophen if needed or medications as prescribed by their health-care provider.
For more details on how to care for your child after sclerotherapy, please see: Sclerotherapy: Caring for your child at home after the procedure.
At SickKids
If you have any questions about the procedure, please call the Image Guided Therapy (IGT) clinic at (416) 813-7654 ext. 201804. Speak to the IGT clinic nurse during working hours or leave a non-urgent message.
For more information on fasting see Eating and drinking before surgery.
For more information on preparing your child for their procedure see Coming for surgery.