What is transposition of the great arteries (TGA)?
Complete transposition of the great arteries (TGA) is a rare congenital heart defect. Congenital means present at birth. It is a common reason for a newborn to have heart surgery.
In a standard heart, the blood low in oxygen comes from the body back to the heart’s right side and is pumped through the pulmonary artery to the lungs where it "reloads" oxygen and goes to the left side of the heart to be sent to the body through the aorta. This way oxygen is distributed to the whole body.
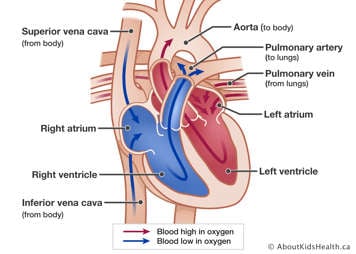
In people born with TGA, the two main arteries (the great arteries) that are connected to the heart are switched, or transposed.
- The aorta is connected to the heart’s right ventricle instead of the left ventricle.
- The pulmonary artery is connected to the left ventricle instead of the right ventricle.
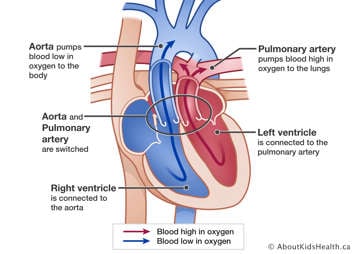
This switch of the great arteries means that blood that is low in oxygen gets pumped around the body instead of blood that is high in oxygen. An open-heart surgery called the arterial switch operation is needed to fix this problem with the heart's arteries.
Some patients with TGA may also have other heart problems, such as a ventricular septal defect (VSD), abnormal coronary arteries (blood vessels that carry blood and oxygen into the heart muscle) or pulmonary stenosis.
How is TGA diagnosed?
TGA can sometimes be detected during pregnancy before a baby is born by routine ultrasound. After birth, if a baby appears blue (cyanotic) and has low oxygen saturations, TGA is suspected. An echocardiogram is done to confirm the diagnosis. Commonly, a chest X-ray and ECG are also performed.
How is TGA treated?
Before the surgery
Before having the arterial switch operation, most babies born with TGA need to be stabilised by increasing the amount of oxygen rich blood that gets to the body before they are ready for the arterial switch operation. This can be done using a medication called prostaglandin and an interventional procedure performed at the bedside called a balloon atrial septostomy.
Prostaglandin given through the vein keeps the arterial duct (PDA) open, which allows blood to mix. This results in more oxygen rich blood getting to the body's organs. This medication can sometimes interfere with a baby's breathing. A ventilator is used to help with the breathing.
Balloon atrial septostomy
For most babies, a balloon atrial septostomy is also required to increase oxygen to the baby’s body. This is a procedure performed at the bedside. It involves putting a catheter (small tube) into a vein in the baby’s leg and passing the catheter into the heart and across the atrial septum (the wall that divides the two upper chambers, or atria, of the heart). A balloon at the end of the catheter is inflated and pulled back across the septum to make a hole.
This hole in the atrial septum allows blood that is high in oxygen in the left atrium to mix with blood that is low in oxygen in the right atrium. The result is that blood higher in oxygen is pumped to the body via the aorta. The hole that is created is fixed at the time of the arterial switch. A balloon atrial septostomy is generally very safe. Prostaglandin can sometimes be stopped after the balloon atrial septostomy.
To read more about this procedure, please see the page Balloon atrial septostomy.
The arterial switch operation
Usually, the arterial switch operation takes place within the first two weeks after being born. If there is a VSD, sometimes this can be delayed to about six weeks old.
The arterial switch operation switches or swaps the great arteries back to their normal position, so that the aorta is connected to the left ventricle and the pulmonary artery to the right ventricle. In addition to swapping the great arteries, the coronary arteries are attached to the new aorta in the correct position. If there is a VSD then that is closed as well.
To read more about this procedure, please see the page Arterial switch procedure.
Complications of the arterial switch
Although the arterial switch is major heart surgery, it is a very successful operation. However, some complications can occur. TGA is a lifelong condition and therefore it is important to keep seeing a cardiologist as many complications can be detected before symptoms develop.
Pulmonary artery and branch pulmonary artery narrowing
In a small number of children, the main pulmonary artery or the branch pulmonary arteries may become narrow. Sometimes an intervention called a balloon dilation is needed to enlarge the narrowed section and, rarely, a stent ( small metal tube) is required to widen the narrowed section by supporting the walls of the blood vessel or conduit to keep it open. If this is not successful, another operation may be required.
Coronary artery problems
Much more rarely, a problem with a coronary artery, which was moved at the time of the arterial switch operation, may develop. A CT scan or cardiac catheterization may be needed to diagnose this problem.
Dilation of the aorta and leaky aortic valve
Sometimes the aorta can dilate (become larger) at the site where it was reattached to the left ventricle, this can be diagnosed by regular follow up with a cardiologist. Similarly, a leaky aortic valve can be diagnosed before symptoms develop.
What is the long-term outlook for children with repaired TGA?
Can patients with a repaired TGA exercise normally?
Children who had surgery for TGA are expected to grow and be able to exercise normally. In the past patients with congenital heart disease were often told not to exercise, or to push too hard during exercise as the heart was weak. However, this is not true and regular exercise is beneficial. People with repaired TGA can usually participate in all sporting activities without restrictions. If this is not the case, your cardiologist will let you know.
Family history and CHD
The risk for any person having a baby with congenital heart disease is about 1%. Babies born to a parent who has congenital heart disease, such as an TGA, the chance that the baby will have any type of congenital heart disease is about 3% . This risk is for both men and women. That still means there is a 97% chance that the baby will not have congenital heart disease.
Women with congenital heart disease can talk with a genetic counselor or genetic specialist before becoming pregnant. A special ultrasound scan of the fetus’ heart can be performed during the pregnancy to look for congenital heart disease.
