What is pyloric stenosis?
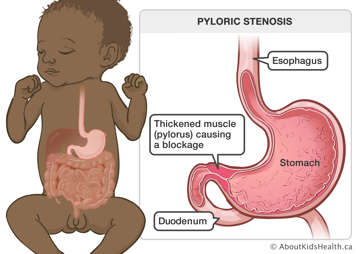
Pyloric stenosis is a blockage of the opening from the stomach to the small intestine. Pyloric stenosis is also called hypertrophic pyloric stenosis. The pylorus is a muscle around this opening. Normally, this muscle keeps food in the stomach when it tightens and lets food out of the stomach when it relaxes. But when the muscle below the stomach is thick and tight, like in pyloric stenosis, it cannot relax properly to allow breast milk or formula through. This means the breast milk or formula you feed your baby cannot pass easily from the stomach to the intestine, which makes your baby vomit (throw up).
How is pyloric stenosis diagnosed?
Pyloric stenosis is diagnosed by ultrasound imaging, along with clinical examination and a careful review of symptoms.
What is a pyloromyotomy?
A pyloromyotomy is a surgery (an operation) to repair the pylorus. During the operation, the surgeon cuts the tight muscle between the stomach and small intestine. This loosens the muscle so the stomach can empty and breast milk or formula will be able to pass easily into the small intestine. This will allow for your baby to feed and grow.
What to bring to the hospital
Your baby will already be staying in the hospital, so you do not need to bring anything for them on the day of the operation. But you may want to bring a toy that is special to your baby. On the day they are released from the hospital, bring your baby's car seat for travel home.
Before the operation
Many babies with pyloric stenosis may be dehydrated and may have electrolyte imbalances in their blood due to vomiting. They will need intravenous (IV) fluids and will require their electrolytes to be corrected before surgery can be performed. They may have a temporary tube inserted through their nose into their stomach (nasogastric tube) to help empty the contents of the stomach and make them more comfortable. During this time, your child will not be allowed to eat.
Your child will remain hydrated with the IV fluids that they are receiving and blood work may be repeated to ensure their electrolytes are within acceptable ranges to proceed with surgery.
Before the operation, you can go with your baby from the inpatient unit to the operating room waiting area. You will then go to the parents'/caregivers’ surgical waiting area until the operation is finished.
During the pyloromyotomy
Before the operation starts, your baby will be given a general anesthetic. This helps make sure your baby sleeps through the operation and does not feel any pain. The surgeon will make a cuts in the pylorus to loosen the muscle. A pyloromyotomy takes about one hour, but your baby may remain in the operating room for a longer period of time for recovery, which is normal.
After the pyloromyotomy
After the pyloromyotomy, your baby will go to the Post-Anesthetic Care Unit (PACU) or recovery room. They will stay there for about one hour. You can visit your baby when they wake up. Your baby will then go back to the inpatient unit for recovery.
Approximately two hours after the surgery, your baby will be allowed to try and feed again. It is common that your baby may still vomit for a short period of time after surgery.
Your baby will have an IV tube in their arm. This gives fluids and medications directly into your baby's blood. The IV will be taken out when it is no longer needed for medications or fluid and your baby is drinking well.
Your baby can go home when all of the following happen:
- their heart rate, breathing, blood pressure and temperature are normal
- they are eating well without excessive vomiting (at least two full feeds with less than 25% vomiting)
- they are comfortable taking pain medication by mouth
This is usually one to three days after the operation.
You should plan to take time off work to take care of your baby
It is difficult to plan how much time you will need to take off work. You should be able to go back to work after about one week.
Caring for your baby at home
Care of the incision
The incision(s)) (surgical cut(s)) from the operation will be covered by a dressing called steri-strips or surgical skin adhesive. You do not need to do anything to the strips or surgical skin adhesive. Wash your hands before touching or cleaning the incision area.
A small amount of blood on the strips is common. If the blood seems fresh (bright red in colour) or if the amount of blood increases, press on the area with a clean, dry washcloth for five to six minutes. Then call your baby's surgeon's office. If the bleeding does not stop, take your baby to their health-care provider or to the emergency department.
The steri-strips or surgical skin adhesive will fall off on their own. If they have not fallen off already, you can take off the strips seven to 10 days after your baby's operation.
Activities
You can allow your baby to do all normal activities once they return home.
Food and drink
During the first 24 hours after the operation, your baby may still vomit. This is common. The vomiting is usually due to the swelling at the surgery site . It will slowly get better.
Your baby should be able to drink breast milk or formula that they normally take, approximately two hours after the operation. They may spit up, which is normal for babies.
If your baby continues to have vomiting that is not getting better, call your baby’s surgeon's office.
Pain medicine
Your baby can have pain medicine as needed after the first 24 hours. This type of operation is usually not very painful, so your baby should only need plain acetaminophen by mouth. Babies younger than six months of age cannot have ibuprofen.
Bathing
You can wash your baby 48 hours after the operation. Avoid submerging the surgical areas in the bath. You can sponge bathe those areas with non-scented soap and water. After two weeks, your baby can have a bath.
When to call the surgical team
The main concerns after a pyloromyotomy are:
- wound infection
- the pyloric stenosis coming back
Call your baby's surgeon's office or return to the emergency department if you notice any of the following signs or symptoms of infection in your baby within one week of discharge:
- fever of 38.5°C (100.4°F) or higher (fever in babies younger than three months always requires a trip to the emergency department)
- thick yellow or green, foul-smelling discharge from the incision area
- bleeding at the incision area
- redness at the incision area
- pain that gets worse, even after taking pain medicine
- swelling at the incision area
- less appetite or vomiting (throwing up)
Another concern is continued vomiting. Please call your baby's surgeon's office or return to the emergency department if you notice any of the following:
- vomiting after most meals
- weight loss
- your baby is not urinating (peeing) as much as usual
- your baby feels lethargic or very tired or drowsy
- your baby has symptoms of dehydration – sunken fontanelle (the soft spot at the top of the baby’s head), sunken eyes, dry lips, crying without tears, etc.
If you have a question or a concern that is not urgent, call your baby's surgeon's office or the General Surgery Clinic during business hours or leave a message on the answering machine after hours. If you have an urgent concern, take your baby to their health-care provider or the nearest emergency department.
At SickKids
The General Surgery inpatient unit is located on the 5th floor, on 5B.
The Operating Room and Surgical waiting area are located on the 2nd floor, as well as the PACU.
The Emergency Department is located on the main floor.
The General Surgery clinic is located on the 6th floor, on 6D. The clinic phone number is (416) 813 7272. The clinic email is generalsurgery.clinic@sickkids.ca.