What can I do to help my child with cancer-related pain?
It is important to understand that how your child thinks, feels or behaves can impact how much pain they have or how well they are able to cope with the pain. For example, if your child is very scared or sad, that can make their pain feel more intense and harder to deal with.
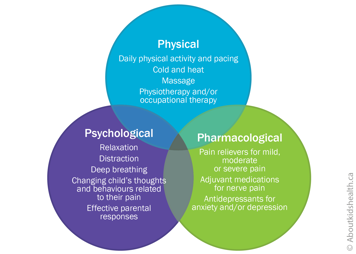
Cancer-related pain treatments often involve a mix of physical, psychological and pharmacological (medication) strategies. Together, these are called the 3Ps of pain control. Like three legs of a stool, the 3Ps are complementary, or supportive, to one another.
Physical strategies
Physical strategies are activities that help the body to function physically. They might include conditioning exercises, stretches and nervous system retraining. For example, graded exercise is a physical strategy that gradually increases the exercise over time, as your child gains strength. These strategies are typically guided by physiotherapists and occupational therapists.
Other ways of reducing pain include using heat, cold, or massage. For instance, the cold sensation from popsicles and ice chips can be really helpful for relieving pain from mouth sores.
Psychological strategies
Psychological strategies can be thought of as "mind-body" strategies or "the power of the brain to help the pain".
In young children, psychological strategies tend to focus on behaviours rather than thoughts about their pain. Examples of behavioural strategies include:
- empowering children to make coping statements (such as "I can get through this")
- encouraging children to keep their regular routines as much as possible
- providing rewards (such as stickers or verbal praise) when they talk to you about their pain or help to manage it, for example by taking deep breaths or medications
For children aged two to five, it can be helpful to comfort them by:
- giving their favourite blanket or comfort object
- distracting them using their favourite toys or by singing their favourite song.
Older children can begin seeking support from others. Encourage an older child to talk to their doctor or nurse when they need support to deal with their pain.
Distraction
Distraction can be a particularly helpful psychological strategy when a child is experiencing pain or having a painful test or procedure. Distract your child with an activity or item that is of interest to them. Active distraction (such as doing an activity or talking with friends) is better than passive distraction (such as watching TV).
Guided imagery
You can help your child use guided imagery to cope with an episode of pain by asking them to imagine that they are in a calm, peaceful environment or to remember a pleasant experience from their past. Encourage your child to describe what they see, as well as any smells, sounds or other sensations. Older children can also listen to online guided imagery scripts.
Relaxation
Relaxation is another psychological strategy that can help your child cope with chronic pain. Belly breathing is one such technique.
Your child’s health-care team may teach you other strategies to support your child and reduce the impact of cancer-related pain on the child and family. These include helping to distract your child from pain, remaining calm and developing a plan in place to cope with pain when it arises.
Pharmacological strategies (medications)
Pharmacological strategies are the medications that treat your child’s pain.
Pain medications are typically divided into the following categories.
Simple analgesics (pain relievers)
Analgesics (medications to lessen the pain) are used to decrease the sensation of pain without causing your child to lose consciousness. Simple analgesics include acetaminophen. They are helpful for mild to moderate pain. If your child has moderate pain, their health care team may use a mix of simple analgesics and a mild opioid medicine (see below). The health-care team will likely tell you to avoid aspirin (acetylsalicylic acid or ASA) and ibuprofen because they can increase your child’s risk of bleeding.
Anaesthetic creams
Anaesthetic creams may be used to numb part of your child’s body if they are having a procedure that involves only the top surface of the skin, such as putting in an IV needle.
Opioids
Also known as narcotics, opioids are generally used for moderate and severe pain. These drugs, which include morphine and hydromorphone, work on the brain by changing how it perceives pain signals. Like most medicines, opioids have side effects. These include slower breathing, sleepiness, nausea, vomiting, constipation, and itchiness. It is important to discuss the benefits and side effects of any drug with your child’s doctor.
You might fear that your child will become addicted to the opioids prescribed to them. Addiction means taking a substance for its mind-altering effects (a "high" or state of euphoria), requiring more medication over time and developing withdrawal symptoms. Opioids are less addictive when they are used properly and your child is closely monitored. Your child’s health-care team will monitor the dose they are given carefully. Once your child’s pain eases, they may require a smaller or weaker dose little by little, but this is only to avoid unpleasant withdrawal symptoms, not because they were addicted.
Sedation
Sedating medications may be used to reduce any fears your child may have before scans or tests that involve needles deeper than the surface of the skin. Sedation uses different combinations of drugs that are given for a short time. This is done in the hospital and your child will be closely monitored.
Adjuvants
Adjuvants are a group of medications shown to work well for pain but are mainly used for other reasons. Examples include anticonvulsants and cannabinoids.
Other medications
Special anticonvulsant medication such as gabapentin may be required if your child has neuropathic pain.
In small doses, certain anti-depressants, such as amitriptyline, can also ease neuropathic pain. Unlike other pain medications, these do not work immediately but instead can take up to 5 days to take effect.
A mouth wash with analgesics can numb tissues in your child’s mouth to give relief from mouth sores before eating or drinking. A bicarbonate mouth wash can help the sores heal and stop them from getting worse.
As with all medications, talk to your child’s health-care team for more information.
If your child is involved in their treatment, share with them the handout Five Questions to Ask About My Medicine. It will help them be better prepared when meeting with their health-care team.




