What is ulcerative colitis?
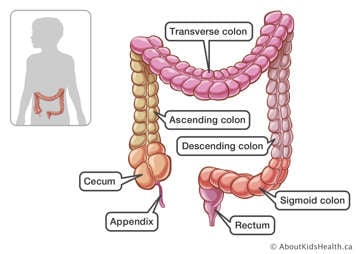
Ulcerative colitis (UC) is a type of inflammatory bowel disease (IBD). UC is a condition that causes inflammation in the colon (also called the large intestine or large bowel) of your gastrointestinal (GI) tract. Inflammation is when part of your body gets red, swollen and painful.
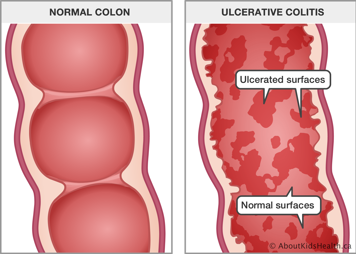
It is important that both words, "ulcerative" and "colitis" be used, when speaking to a health-care provider. The term ulcerative is used because there are small breaks, called ulcers, in the lining of the colon when the disease is active. Colitis refers to inflammation of the colon. When a child has active UC, symptoms like diarrhea, rectal bleeding and abdominal pain can result.
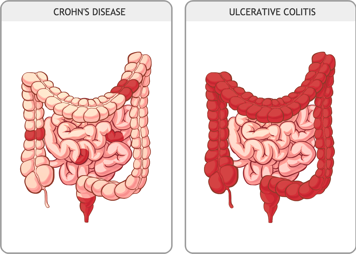
The other main type of IBD is called Crohn's disease (CD). CD and UC are very similar, but are not exactly the same. In CD, inflammation can happen anywhere along the GI tract, from the mouth to the anus. Symptoms depend on which part of the GI tract is inflamed. Your child's health-care provider will ask questions and perform certain tests in order to tell the difference between CD and UC and will suggest treatments based on which form of IBD is diagnosed. You can get either type of IBD at any age.
There are over 6,200 children under 18 years old in Canada with IBD right now, and the number of new diagnoses is rising most quickly in children under 6 years old (very early onset IBD [VEOIBD]). When it is too difficult to tell whether a patient has CD or UC, their IBD is classified as IBD-U. The "U" stands for unclassified; IBD-U may also be called indeterminate colitis.
Where does ulcerative colitis happen?
UC occurs mostly in the colon. Sometimes the stomach can also be affected. In UC, inflammation in the colon is continuous. This means that ulcers occur consistently in part of the colon. UC can occur as pancolitis (the entire colon), left sided (rectum, rectum to sigmoid or rectum to descending colon) or right sided (ascending colon). Knowing your child’s symptoms and where the inflammation is can help you and the health-care team choose the right treatment.
What does ulcerative colitis feel like?
Someone with UC can have many different symptoms, like stomach pain, diarrhea, blood passed from the anus, urgency to go to the bathroom, weight loss, fatigue and decreased appetite. They can less commonly have fevers, joint pain, certain skin rashes and redness of the eyes. Some people may have just a few of these symptoms while others may experience them all.
UC is a chronic condition; this means that it is for life. Although there is currently no cure, there are a lot of treatment options. When you find one that helps to keep your child’s UC under control, they can be in remission for a long time (that means the inflammation and ulcers have healed and your child is "symptom-free").
What causes ulcerative colitis?
Even though there have been many scientific studies, researchers do not yet know what causes UC. They do know that it can run in families. You are more likely to get UC if one of your first-degree relatives, such as a brother or sister, has it. You are even more likely to get it if that brother or sister is your identical twin. Anyone can get UC at any age. In children, it occurs slightly more often in boys. In teens, it occurs more often in girls.
Researchers think UC is caused by:
- Genetics: Some people may have genes in their body that increase their chances of getting CD. Studies have shown that there are over 200 genes that may be linked with IBD, but most of those genes only increase your risk a small amount. So other factors are needed to get the disease. Very young children with VEOIBD can sometimes have a single gene causing their IBD (called monogenic IBD), which requires very specialized care.
- Environment: Our environment includes anything our body comes in contact with. Exposure to antibiotics early in life, and living in a city are the most well-known types of environmental "triggers" that may contribute to IBD, but there are probably others.
- Immune system: Our immune system protects us from harmful bacteria and viruses, but in some people, it can cause inflammation in the body (such as in the GI tract).
- Gut microbiome: Lots of bacteria live in your guts and the types of bacteria may change your risk of getting IBD.
- A combination of all these: The most common theory is that you need a combination of all the above things to get UC. For example, in people with the genes for IBD, certain environmental factors change the gut microbiome early in life, which triggers the immune system to respond later in life, causing IBD.
What kinds of treatments are there?
There are six classes of medications used to treat the symptoms of UC. These medications can come in the form of pills, liquids, intravenously (through a vein), injections and suppository or enema. Check with your child's health-care provider to learn more about their medications. Some people might also consider UC surgery.
The different types of medication used to treat UC are:
- 5-aminosalicylic acid (5-ASA): Used for mild to moderate forms of UC, 5-ASA decreases inflammation in the intestinal tract. It can be taken orally (by mouth) or rectally (in the anus/rectum).
- Immunomodulators: Used for long-term treatment, these drugs work by suppressing the immune system to help reduce inflammation. Immunomodulators may also help patients stay in remission. They are not intended for acute flare-ups. Immunomodulators are given orally.
- Steroids: These drugs are used for moderate-to-severe UC for a short period of time to help decrease the amount of inflammation in the body. They can be taken orally, intravenously or rectally.
- Antibiotics: Antibiotics are sometimes used for UC patients who have an infection (such as C. difficile), or in addition to other medications to make them work better. They can be given orally or intravenously.
- Biologics: These medications act against specific chemicals (cytokines) in the body to reduce inflammation. They are often administered intravenously or subcutaneously (with a needle under the skin).
- Small molecules: These medications also act against chemicals that cause inflammation but are given orally. These medications are not approved for use in children by Health Canada, but are sometimes available for some children who need them.
Sometimes when medications are not working to treat the inflammation, surgery is done to remove the colon in a procedure called a ‘colectomy’, leaving a temporary ostomy bag. Often the small bowel can be attached back to the rectum at a later date.
Recommended resources:
- SickKids IBD Centre website: https://www.sickkids.ca/en/care-services/centres/inflammatory-bowel-disease-centre/
- Crohn’s and Colitis Canada: https://crohnsandcolitis.ca/
- GI Kids org (website for parents from the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition): https://gikids.org/inflammatory-bowel-disease/
- Your Child With Inflammatory Bowel Disease (Book): https://a.co/d/91fLoJF
