What causes acute pain in older children?
In older children (ages six to 12), common causes of acute pain include:
- routine vaccinations by needle
- earaches and sore throats
- injuries from everyday physical activities
- dental treatments such as cavity fillings
- procedures such as blood work, lumbar punctures or intravenous starts
- surgeries (operations)
- complex health conditions such as cancer or juvenile arthritis
Assessing acute pain at home
Older children can usually "self-report" their pain (describe it in their own words or rate how bad it is) rather than have a parent or health-care professional speak for them.
One reason is that they can use specific pain words (such as "aching", "burning" or "stabbing") to better explain their experience and where exactly in the body their pain is coming from. Older children can also start reporting what can make their pain better or worse.
But it is important to remember that children at the younger end of this age group may be too fearful or stressed to self-report their pain accurately.
Assessing acute pain in medical settings
At this age, it is usually best for a child who can talk about their pain to self-report it in the hospital.
Most children in this age group can rate their level of pain using pain scales. Children around the age of six may use words like "small", "medium" or "a lot" to rate their pain or be able to use a picture pain scale such as the Faces Pain Scale - Revised.
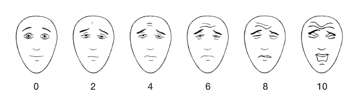
Older children in this group can use numeric rating scales, for example by verbally rating their pain from 0 to 10, where 0 is 'no pain' and 10 is the worst or strongest pain they can imagine. With repeated use, these scales can reveal if your child's pain is changing (getting better or worse) over time.
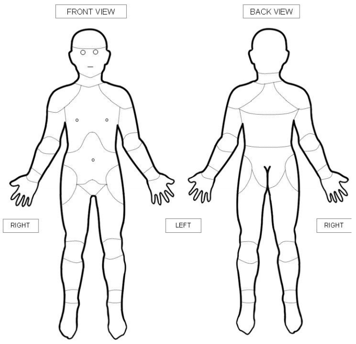
Body diagrams can also be helpful tools for assessing an older child's pain. Older children can point at the diagram and share exactly where they are feeling pain in their body.
Factors affecting pain assessment
A developmental disability or intellectual disability may make it difficult for your child to express their pain in words. In this case, their health-care team will use standard pain assessment tools to look at their behaviour. One such tool is the NCCPC, which helps make caregivers more aware if a child's behaviour may be different than usual due to pain.
Gender can affect how children express pain and how accurately their pain might be assessed. For instance, older boys may put a lot of effort into making sure they do not cry, especially if others are around. On the other hand, young girls may cry more because this behaviour is deemed more acceptable in some cultures. Or, the opposite may happen. It is important to ask a child about their pain and not make assumptions based on gender or sex.
Cultural differences can also account for a wide variety of reactions to situations. Some cultures may express themselves freely, but others may repress their emotions or respond to pain in unexpected ways. Some children may adopt the role of a "good patient" and behave the way they believe health-care professionals want them to behave rather than express how they are feeling.
How you can help health-care professionals understand your child's pain
No matter how old your child, it is important to ask about their pain and help them feel safe to truthfully express how much pain they are feeling. Your child's self-report is essential for health-care providers to give the most accurate assessment and recommend the most appropriate treatment.
If your child cannot speak for themselves, it is also important that you tell the health-care team how you know if your child is in pain.
Websites
Faces Pain Scale-Revised
https://www.iasp-pain.org/Education/Content.aspx?ItemNumber=1519
Distraction toolkit
https://www.childrenshealthcarecanada.ca/en/networks-and-hubs/Pediatric-Pain/FINAL_Distraction_CAPHC_Powerpoint-Presentation.pdf
Reducing the pain of vaccination in children and teens (PDF)
https://immunize.ca/sites/default/files/Resource%20and%20Product%20Uploads%20(PDFs)/Products%20and%20Resources/Pain%20Management/Parents/painreduction_kidsandteens_web_22_e.pdf
Managing your child's pain from braces
https://blog.1stfamilydental.com/reducing-braces-pain/
Managing your child's pain from sports injuries
https://www.stanfordchildrens.org/en/topic/default?id=tackling-kids-sports-injuries-1-4288
Preparing your child with cancer for painful procedures
https://www.cancer.net/navigating-cancer-care/children/preparing-your-child-medical-procedures
Videos
Pain management at SickKids (2 mins 49 secs)
https://www.youtube.com/watch?v=_9_OQFo2APA
Reducing the pain of vaccination in children (Centre for Pediatric Pain Research) (2 mins 18 secs)
https://www.youtube.com/watch?v=KgBwVSYqfps
Reducing the pain of vaccination in children (Dr. Taddio) (20 mins 52 secs)
https://www.youtube.com/watch?time_continue=2&v=TGGDLhmqH8I
Learning how to manage pain from medical procedures (Stanford Children's Health) (12 mins 58 secs)
https://you.tube/UbK9FFoAcvs
Content developed by Rebecca Pillai Riddell, PhD, CPsych, OUCH Lab, York University, Toronto, in collaboration with:
Lorraine Bird, MScN, CNS, Fiona Campbell, BSc, MD, FRCA, Bonnie Stevens, RN, PhD, FAAN, FCAHS, Anna Taddio, BScPhm, PhD
Hospital for Sick Children
References
Gold, J.I., Mahrer, N.E. (2017) Is Virtual Reality Ready for Prime Time in the Medical Space? A Randomized Control Trial of Pediatric Virtual Reality for Acute Procedural Pain Management. Journal of Pediatric Psychology, 2017; https://academic.oup.com/jpepsy/article/43/3/266/4558507
Hicks, C.L., von Baeyer, C.L., Spafford, P., van Korlaar, I., Goodenough, B. (2001). The Faces Pain Scale - Revised: Toward a common metric in pediatric pain measurement. Pain 2001;93:173-183.
McMurtry, C.M., Chambers, C.T., McGrath, P.J., & Asp, E. (2010). When "don't worry" communicates fear: Children's perceptions of parental reassurance and distraction during a painful medical procedure. Pain, 150(1), 52-58.
Uman, L.S., Birnie, K.A., Noel, M., Parker, J.A., Chambers, C.T., McGrath, P.J., Kisely, S.R. (2013) Psychological interventions for needle-related procedural pain and distress in children and adolescents. Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.CD005179.pub3
Taddio, A., McMurtry, C.M., Shah, V., Pillai Riddell. R. et al. Reducing pain during vaccine injections: clinical practice guideline. CMAJ 2015. https://doi.org/10.1503/cmaj.150391
von Baeyer, C.L. (2009). Children's self-report of pain intensity: what we know, where we are headed. Pain Research and Management, 14(1), 39-45.
