What is a Chiari malformation?
A Chiari (say: key-AR-ee) malformation is when the lower part of the brain sits too low in your child's upper spine (neck) area.
There are several types of Chiari malformation. Type 1 and type 2 are the most common:
- Type 1 is when a part of the brain called the cerebellar tonsil sits too low in the upper spine area. Children with type 1 Chiari malformation rarely have any symptoms, but they may have headache, neck pain or signs of a syrinx and/or scoliosis (curvature of the spine).
- Type 2 is when the lower part of the brain (the brainstem) sits too low. This page mainly discusses type 2 Chiari malformation.
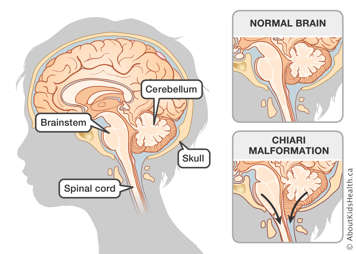
The brainstem controls important body functions such as breathing, heartbeat, and swallowing. When it is lower than usual, the brainstem can be compressed or squished with the upper part of the spinal cord. This means that your child may have problems such as the following:
- trouble breathing
- slow heart rate
- choking, gagging or other trouble swallowing
A Chiari malformation can also block the cerebral spinal fluid (CSF) from traveling in and around the brain and spinal cord. CSF is an important fluid that provides food for the brain and spinal cord. CSF also acts like a shock absorber to protect the brain and spinal cord from injury.
What is a syrinx?
Sometimes, when the flow of CSF into the spine is blocked, a syrinx is formed. A syrinx (say: SEAR-inks) is a small cyst or pocket of fluid that forms when some CSF becomes trapped inside the spinal cord. Often, fixing the Chiari malformation can help fix the syrinx.
Chiari malformation causes different symptoms
Some of the symptoms your child may have include the following:
- Headache.
- Increased sensitivity to things in the mouth. For example, your child may gag when they brush their teeth.
- Gagging or choking on food or drinks. If this is severe, food or liquid may enter the lungs. This is called aspiration.
- In babies, a weak suck when feeding.
- Change in your child's voice or cry. Babies may have a weak cry. Some children may have stridor, which is a high-pitched "croupy" sound, when they cry.
- Weakness in the arms or hands.
- Pain, tingling or other abnormal feelings in the neck, arms or hands
- Snoring, trouble breathing or changes in breathing pattern. If this is severe, your child may stop breathing for more than 15 seconds. This is called apnea.
- Tendency to arch head back.
What causes a Chiari malformation is not known
Type 2 Chiari malformations are found in many children with spina bifida. But having a Chiari malformation does not always mean your child has spina bifida.
Chiari malformation is diagnosed with an MRI scan
Your doctor will arrange for a test called an MRI scan. An MRI scanner is a machine that can take special pictures of your child's brain. It will show where your child's brainstem is sitting and if it is compressed or squished. This test will tell the doctor if your child has a Chiari malformation. An MRI of your child's spine may also be done to look for evidence of a syrinx.
MRI requires your child to stay still while the pictures are being taken. Some children need sedation medicine to help them keep still during the tests.
Your child may need an operation
Your child may need surgery (an operation) to repair a Chiari malformation. The surgery involves giving the brainstem more room so it is no longer compressed.
The surgery is referred to as a "Chiari decompression" or a "posterior fossa decompression." The area at the bottom of the brain and top of the spinal cord is also called the posterior fossa area.
What happens during the operation
Your child will be given a special "sleep medicine" called a general anesthetic to make sure they sleep through the operation and do not feel any pain.
The surgeon will cut in a vertical (up and down) line at the back of your child's neck. The cut will start at the bottom part of the skull and extend down to the top part of the neck. Then the surgeon will remove small pieces of bone from the bottom of your child's skull and the top of the spine to give the spinal cord more room.
The surgery is usually about three or four hours long, but it may take longer.
Your child will stay in hospital for about five to seven days after the surgery
Depending on how your child is doing, they may spend the first night after surgery in the intensive care unit, or they may be cared for in the close observation room on the neuroscience unit. Your child will probably need to stay in hospital for about five to seven days in total.
Your child will have medicine to help with pain
Your child may feel pain at the operative site. Usually, your child will have morphine through their intravenous line (IV) for one or two days. This should control the pain. If it does not control the pain, speak to your child's nurse.
After one or two days, the morphine drip will be slowed down and your child will take pain medicine by mouth.
Your child may also learn other ways to control pain, such as blowing bubbles or relaxation breathing. Ask your nurse or the Child Life specialist to help you and your child learn how to do this.
Your child may have monitors attached
Your child may need to have monitors attached. Monitors are machines that help the nurses keep track of the following:
- your child's breathing
- your child's heart rate
- if your child is getting enough oxygen
Your child will probably be sore after the surgery
The back of the neck has a lot of muscles, so after the surgery, your child may have a sore neck. They may find it hard to move their head.
A physiotherapist may be involved in your child's care. The physiotherapist will give your child exercises to help the neck muscles recover after surgery.
Going home
Before you take your child home, the surgeon or the nurse will explain how to take care of your child at home. The instructions will include the following:
- how to take care of your child's incision (cut)
- what to do with your child's stitches or staples
- how to tell if your child's incision becomes infected
- other things to watch for
Taking care of your child's incision
Watch your child's incision (cut) to make sure it is healing well. It is all right if the incision gets wet in the bath or shower. Your surgeon and a nurse will discuss with you how long to wait before your child can have a bath or shower.
Taking care of your child's stitches
How your child's staples or stitches are taken out depends on the type of staple or stitch that was used. Your surgeon or nurse will tell you what type of stitches were used.
- If your child has staples or stitches that need to be taken out, your family doctor will need to do this. The stitches should be taken out about seven to 10 days after the operation. Staples should be removed about 10 days after the operation. Your surgeon or nurse will tell you when they need to come out.
- If staples were used, you will be given a special remover to take to your family doctor.
- If your child has the kind of stitches that dissolve on their own, you can see your family doctor to have the incision line checked, but the stitches will not need to be taken out.
How to tell if your child's incision is infected
Tell your surgeon if you notice any of the following signs of infection:
- fluid leaking out of the incision
- fever
- redness
- swelling
- smelly discharge
- neck stiffness
Other symptoms to watch for
In some cases, the decompression surgery may not work. Watch your child for returning symptoms or new symptoms of Chiari malformation, even after your child goes home. These include:
- headache
- bogginess or fluid collection at the incision site
- vomiting
- irritability
- increased sensitivity to things in the mouth, such as gagging when brushing teeth
- gagging or choking on food or drinks
- in babies, a weak suck when feeding
- change in your child's voice or cry
- weakness in the arms or hands
- pain, tingling or other abnormal feelings in the neck, arms or hands
- snoring, trouble breathing or changes in breathing pattern
- tendency to arch head back
If you notice any of these symptoms, contact your child's surgeon right away.
Following up after the operation
The surgeon will see your child in a follow-up clinic visit about six weeks after your child goes home. The appointment may be made for you when your child is discharged. If not, call the neurosurgery clinic to make an appointment.
Write down the date and time here: