How can I tell if my child has cancer-related pain?
No medical test can tell us how much pain a child is experiencing. Instead, parents/caregivers and the health-care team rely on a child’s behaviour and what a child say about their own pain (self-reporting).
Assessing cancer-related pain at home
As a parent or caregiver, you play a crucial role in assessing if your young child is in pain. Watch for any changes in your child’s behaviour and listen to what they say about their pain.
Behavioural signs of pain
- Pained facial expressions, such as grimacing or wincing
- Guarding or protecting part of the body
- Not following usual sleep or eating routines
- Avoiding activities that are usually enjoyable, such as playing with toys, singing songs
- Avoiding school, outings or mixing with other children
- Avoiding physical activity that may provoke pain, such as walking, climbing stairs, hopping, jumping or sports
- Regressing in development, for example needing help with dressing or bathing or wanting to sleep with a parent
Verbal signs of pain
Depending on your child’s age, they may also be able to express their pain with words.
- Very young children (such as two-year-olds) may use simple pain words such as "ouchie", "boo boo" or "hurt" while pointing to or protecting the part of the body that is in pain.
- Through ages three and four, most children gradually learn to describe around four levels of pain intensity ("none", "a little", "some or medium" and "a lot").
- When a child is aged four or five years, they are even better able to express their pain verbally, but they might still confuse different types of hurt (for instance physical pain and hurt feelings).
- Children aged six to 12 may complain about their pain directly, but others may be able to localize (pinpoint) the pain in their body.
It is important to separate the signs of physical pain and emotional distress, especially if your child is not yet verbal or has more limited language abilities. To see if your child’s pain is mainly physical, watch for the behavioural signs listed above. To assess if your child is in distress, think about any recent events that may be affecting them, such as changes in their school, daycare or living arrangements, separation from a caregiver or illness or death of a family member.
Even though it is important to recognize the difference between physical pain and emotional distress, it is also important to let children know that you believe their pain is real.
Questions
What would a doctor or nurse ask about?
- When and how the pain started, where it is located, what words would describe the pain, how strong the pain is
- Impact of pain on your child’s sleep and schooling
- Any allergies or other conditions that your child might have or any conditions that run in the family
- If your child is taking medications for pain or other conditions
What would a psychologist ask about?
- Any changes in your child’s behaviour and how much these reflect pain or emotional distress
- How your child’s emotional state might be impacting their pain (for example frustration about missing a favourite activity, which could lead to muscle tension and, in turn, increased pain)
- Your child’s behaviours and thoughts related to the pain (for example avoiding eating because of a stomach ache or thinking the pain will never go away)
- Which coping strategies you or your young child might already use
- How you as a parent or caregiver are responding to your young child’s pain
In some cases, the symptoms of cancer-related pain can be amplified by psychological distress, such as that caused by the disease. The term for this is somatization.
What would a physiotherapist ask about?
- Where in the body your child experiences pain
- How pain is limiting your child’s physical activities
- Which physical treatment approaches your child has used in the past to manage pain (see below)
Physiotherapists would also usually examine your child to assess their quality of movement, strength, range of motion and sensations (for example over-sensitive or under-sensitive to touch).
Assessment tools
Your child’s health-care team will use a range of assessment tools to measure your child’s pain.
One tool that measures your child’s behaviours in relation to their acute pain is the Face, Legs, Activity, Cry, Consolability (FLACC) scale. This scale is used in children aged 2 months - 7 years. It asks parents to recall a time when they know their child was in pain to:
- Describe the child’s behaviours at that time (for example their facial expressions, level of activity and how easily they could be comforted)
- Link those behaviours with numbers from 0-3 for mild pain, 4-6 for moderate pain and 7 or greater for severe pain.
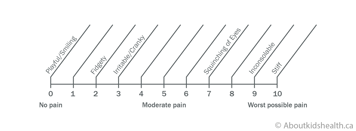
The Individualized Numeric Rating Scale (INRS) is another tool designed for children aged 7 years and older. The child is asked to assign a number to his/her pain with 0 representing no pain/hurt and 10 representing the worst pain ever. The child is then asked how much pain/hurt they are having right now.
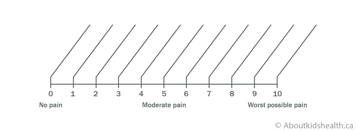
When the behavioural information is filled in, a unique numerical pain scale is created for each child. Healthcare professionals can refer to this scale to assess a child’s level of pain (based on their behaviours) at a given point in time.
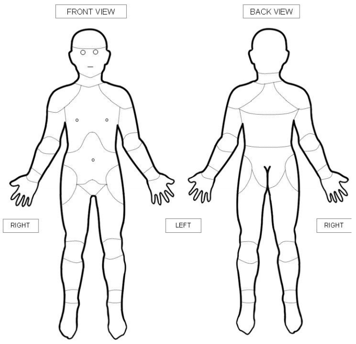
Young children can also report their level of pain by pointing at body diagrams to indicate where in their body they are feeling pain.