Chronic pain treatments involve a mix of psychological, physical and pharmacological (medication) strategies. Together, these are termed the 3Ps of pain control. Like three legs of a stool, the 3Ps are complementary, or supportive, to one another.
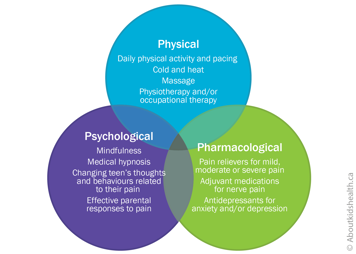
No single strategy will likely be the answer, so it is important to be open to a variety of options if your teen has chronic pain.
Physical strategies
Physical strategies are activities that help the body to function physically. They include conditioning exercises, stretches, endurance activities and nervous system retraining. They are typically guided by physical and occupational therapists.
Pacing is one strategy that can help a teen stick to their routines. It involves learning how to balance activity and rest so that your teen can do important everyday activities (such as participating in school and meeting up with friends) even if they are in pain.
Try using the traffic light analogies below to help your teen follow their routines without making their pain worse.
Pacing guidelines for physical activity
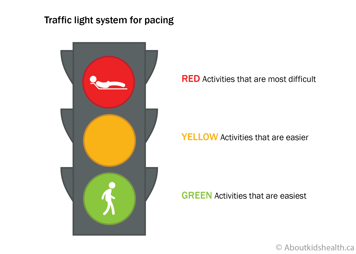
- Red light
- Severe pain increases during an activity and stops activity participation
- Pain persists for days to weeks
- Possible risk of injury
- Yellow light
- Safe pain
- Pain spikes but is tolerable during an activity and will not cause harm
- Pain persists for 24 to 48 hours after an activity before returning to baseline
- Green light
- Safe pain
- Pain spikes but is tolerable during an activity and will not cause harm
- Pain is no worse after an activity
Your teen should stay in the green light and may edge into the yellow. They should not go in the red light.
Pacing guidelines to balance activity and rest
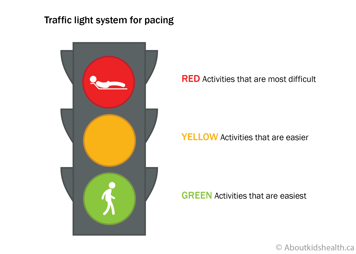
- Red light
- Stop and rest.
- Key phrase: “I need to take a break. I can use my coping strategies for relaxation and recovery so I am ready to go again after my rest.”
- Yellow light
- Be alert.
- Key question: “Am I overdoing it or can I use my coping strategies to keep going a bit longer?”
- Green light
- Be active, but save some of your energy.
- Key phrase: “I am being active and I am fine.”
Your teen should make sure they spend time in the green and red traffic light areas. Yellow reminds them to stop and take a break.
Golden rules of pacing
Understand that it takes time to learn how to pace properly – don’t expect immediate success.
Encourage your teen to try using a timer to know when to stop an activity before their pain or tiredness gets bad.
Encourage your teen to use time as their guide so that they, not their pain, stays in control of their activities.
Remind your teen that they are only pacing themselves, not competing with any of their peers.
Encourage your teen to plan their activities carefully so that they do not squash everything into one day.
Psychological strategies
Psychological can be thought of as "mind-body" strategies or "the power of the brain to help the pain".
They can include therapies to:
- reduce fearful thoughts about pain
- reduce fear of moving a painful area of the body
- decrease stress
- improve confidence in being able to get back into routines and activities that pain has disrupted (such as sports, school, sleep or social activities).
They also include some of the following techniques to support your child and reduce the impact of pain on the family.
Distraction
Distraction can be a particularly helpful psychological strategy when a teen is experiencing pain. Active distraction (such as doing an activity, talking with friends or playing a video game) is better than passive distraction (such as watching TV).
Guided imagery
Your teen can use guided imagery to cope with an episode of pain by imagining that they are in a calm, peaceful environment or remembering a pleasant experience from their past. Guided imagery works best when the scene includes what they see, as well as any smells, sounds or other sensations. There are many online guided imagery scripts that your teen can follow on their smartphone or other mobile device.
Relaxation
Relaxation is another psychological strategy that can help your teen cope with chronic pain.
Belly breathing is one such technique, as it helps your teen slow down their breathing and become more relaxed. Encourage them to take a few slow deep breaths into their belly, breathing in through their nose and out through their mouth.
Your teen can place their hands over their belly to check that it is rising with every in-breath and falling with every out-breath.
Behavioural therapy
If your teen has become fearful of moving their body and is very distressed about their pain, they may need specialized therapy to help them. Cognitive behavioural therapy (CBT) can help change a person's unhelpful thoughts and behaviour patterns if they are getting in the way of their day-to-day life. Working with a therapist, your teen can develop strategies and tools to understand and change their unhelpful thinking patterns or behaviours. For example, instead of thinking “I won't go out with friends because I will be a burden to them”, CBT can help someone develop more helpful thoughts such as, “I won’t be able to do the same level of activity as my friends right now, but that doesn’t mean we can’t have fun together. I can invite them over to watch a movie or we can meet up for dinner.”
Pharmacological strategies (medications)
Pharmacological strategies are the medications that treat your child's pain. They are rarely used alone; they should nearly always support physical and psychological strategies.
Pain medications are typically divided into:
- simple analgesics (pain relievers)
- opioids
- adjuvants
Simple analgesics include acetaminophen and ibuprofen. They are helpful for mild to moderate pain (especially resulting from tissue inflammation).
Opioids are among the strongest pain relievers and are often used after surgery or other major painful procedures. If your child is in moderate to severe pain, their health-care team may prescribe opioids such as morphine, oxycodone or hydromorphone for short-term use.
| Opioids have risks and side effects, which can be serious. Always talk to your child's health-care provider for advice on taking, storing and disposing of opioids safely. |
Adjuvants are medications that are shown to work well for pain but are mainly used for other reasons. Examples include anticonvulsants and cannabinoids.
For all medications, talk to your health-care professional for more information.
What kind of improvements should I see in my teen's chronic pain?
Your teen's chronic pain will not always improve consistently. There may be good days and bad days, good weeks and harder weeks.
Sometimes things might even get worse before they get better. For example, as your teen begins their therapies and their body becomes more active, they may experience muscle soreness and throbbing. This is natural in weak or tight muscles that are not used to exercise or stretching and will ease in time.
To stay focused on managing pain effectively, make weekly goals with your teen and remember that improvement can sometimes take time.
Improvements in function
One important area for goal setting is return to function. This means returning to activities that pain has disrupted, for example going to school, taking part in family routines or doing physical or social activities.
A return to function, rather than improvement in pain, is actually the first sign that chronic pain treatment is successful. This is because pain can often take weeks to months to improve while weak muscles gradually become stronger. If your child waits for their pain to go away before getting back into life, there is a risk that their pain will get worse.
Websites
Website designed to help children get control of their pain (German Paediatric Pain Centre)
http://www.deutsches-kinderschmerzzentrum.de/en/
Website where children can learn the Canadian 24-Hour Movement Guidelines the fun way
https://www.participaction.com/the-science/benefits-and-guidelines/children-and-youth-age-5-to-17/
Page designed for children and youth to discuss their medication with their health-care provider
Five Questions to Ask About My Medicine
Videos
How does your brain respond to pain
https://www.youtube.com/watch?v=I7wfDenj6CQ
Seven video mini-series on chronic pain and its management for youth (Pain Bytes)
http://www.aci.health.nsw.gov.au/chronic-pain/painbytes
Module: Understanding different types of pain
https://mycarepath.ca/course/understanding-different-types-of-pain
Module: Importance of getting started on the road to recovery
https://mycarepath.ca/course/importance-of-getting-started-on-the-road-to-recovery
Teenagers talk about their chronic pain (longer video)
https://www.youtube.com/watch?v=56aWuEt4NA0
Teenagers talk about their chronic pain (shorter video)
https://www.liveplanbe.ca/real-stories/growing-up-with-pain/ryans-story
Content developed by Danielle Ruskin, PhD, CPsych, in collaboration with:
Anne Ayling Campos, BScPT, Fiona Campbell, BSc, MD, FRCA, Lisa Isaac, MD, FRCPC, Jennifer Tyrrell, RN, MN, CNeph
Hospital for Sick Children
References
Coakley, R., & Schechter, N. (2013). Chronic pain is like… The clinical use of analogy and metaphor in the treatment of chronic pain in children. Pediatric Pain Letter, 15(1), 1-8.
Coakley, R. (2016). When Your Child Hurts: Effective Strategies to Increase Comfort, Reduce Stress, and Break the Cycle of Chronic Pain. Yale University Press.
Carney, C., Carney, C. E., & Manber, R. (2009). Quiet Your Mind & Get to Sleep: Solutions to Insomnia for Those with Depression, Anxiety, Or Chronic Pain. New Harbinger Publications.
Mayo Clinic: Understanding Pain (http://www. mayoclinic.org/understanding-pain/art-20208632?pg=1)
Mindell, J. A., & Owens, J. A. (2003). Sleep problems in pediatric practice: clinical issues for the pediatric nurse practitioner. Journal of Pediatric Health Care, 17(6), 324-331.
Paruthi, S., Brooks, L. J., D'Ambrosio, C., Hall, W. A., Kotagal, S., Lloyd, R. M., ... & Rosen, C. L. (2016). Recommended amount of sleep for pediatric populations: a consensus statement of the American Academy of Sleep Medicine. Journal of clinical sleep medicine: JCSM: official publication of the American Academy of Sleep Medicine, 12(6), 785.
Valrie, C. R., Bromberg, M. H., Palermo, T., & Schanberg, L. E. (2013). A systematic review of sleep in pediatric pain populations. Journal of developmental and behavioral pediatrics: JDBP, 34(2), 120.