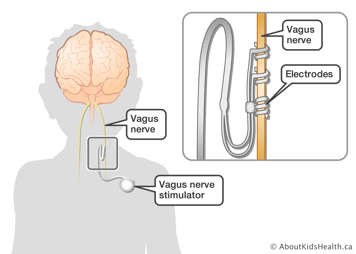
The vagus nerve is one of 12 cranial nerves that pass information to and from the brain. Intermittent (on and off) electrical stimulation of the vagus nerve seems to reduce or prevent seizures.
Vagus nerve stimulation involves performing surgery on your child to implant an electrical pulse generator in their chest and attach electrodes to the vagus nerve in their neck.
How does vagus nerve stimulation work?
A pulse generator is similar to a pacemaker. It weighs about 25 grams (g) and is programmed to intermittently transmit small electrical signals through a wire to the vagus nerve in the neck.
We do not understand why electrical stimulation of the vagus nerve prevents seizures. It may be related to changes in the brainstem and thalamus, or the stopping of abnormal brain activity associated with seizures.

The pulse generator functions automatically 24 hours a day. An external programming wand and software are used by the doctor to read and alter the stimulation strength and frequency.
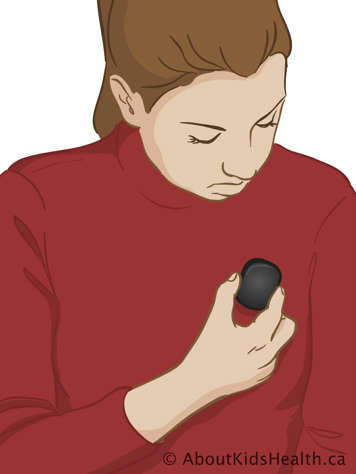
Patients are also given a magnet that acts as a switch for the generator. For some people, this extra stimulation can stop a seizure from progressing, shorten a seizure or reduce the intensity of the seizure. The magnet can also be used to turn the stimulator off temporarily.
The battery life of the pulse generator is about six years, after which it can be replaced. This will require a second operation on your child, similar to the first.
What and who is vagus nerve stimulation best used for?
Vagus nerve stimulation is considered if:
- anti-epileptic medication does not control seizures effectively
- a child is not a good candidate for brain surgery, either because of high risk or because they have various epileptogenic (seizure-generating) areas in their brain
- the neurologist and surgeon decide that a child is large enough to support the implant.
Vagus nerve stimulation should not be used in children with certain cardiac, respiratory or gastrointestinal problems. The vagus nerve serves the heart, lungs and stomach, and some existing problems in these areas may lead to complications with vagus nerve stimulation.
Vagus nerve stimulation usually reduces seizures but does not often eliminate them completely. Usually it is used with medication.
What is the procedure?
Once it has been decided that your child may be helped by vagus nerve stimulation, the surgeon, anaesthetist and others on the medical team will explain the procedure to you in detail. With the help of the treatment team, you should then explain the procedure to your child and help them understand what to expect after the implantation.
Your child will need to be admitted into the hospital for surgery to fit the device. Your child will probably need to be put to sleep under general anaesthetic, and so will need to stop eating eight hours before. The operation can be done with a local anaesthetic, but because it is hard for children to stay still, most require a general anaesthetic.
The procedure itself takes about one hour. One cut about 5 cm long is made on the left chest wall to implant the pulse generator. Another cut about 5 cm long is made in the neck, through which flexible platinum electrodes are attached to the vagus nerve. Because the vagus nerve also goes to the heart, the generator will be turned on in the operating room so that the surgeon can make sure the device does not interfere with the heart. For the same reason, the electrodes are almost always placed on the left vagus nerve, which has less critical influence on the heart.
Your child may be sent home on the same day or kept overnight for observation. You and your child will be taught how to care for the incisions before discharge.
What are the risks of vagus nerve stimulation?
Doctors, family, and your child (if they are old enough) need to discuss the risks and benefits and weigh them against each other before deciding on surgery.
Before the operation, the surgeon will talk to you about the possible risks of your child's procedure. There are some physical changes your child will feel that will get better in time. More serious complications are very rare. Your child will be closely monitored after the operation to watch for any signs of complications developing, and they will be treated immediately.
Surgical risks
All surgeries, and indeed all invasive procedures, have some level of risk associated with them. There are risks from anaesthesia and a risk of infection, bleeding (haemorrhage) and fluid build-up (edema). The anaesthetist, surgeon and care team will take precautions to ensure that these risks are as small as possible, and to treat these complications if they arise.
Lack of effect
Sometimes, despite careful pre-surgical evaluation, the vagus nerve stimulator may not eliminate or reduce seizures. This may occur in about one third of cases.
What are the side effects of vagus nerve stimulation?
The most common side effect of vagus nerve stimulation relates to the voice. The vagus nerve runs close to the nerve that controls the vocal cords. When the stimulator is turned on, the child's voice sometimes sounds hoarse or different than usual. When the stimulator is turned off, the child's voice returns to normal.
Other possible side effects include pain, coughing, tingling over the left side of the neck, shortness of breath, stomach upset, nausea and, more rarely, increased drooling.
Some side effects only occur during stimulation and some may be present throughout. Some problems may only happen at first and will reduce as the body gets used to the device.
What are the potential benefits of vagus nerve stimulation?
One potential benefit is obviously a reduction in seizures. Positive side effects include improved alertness, memory, mood, verbal communication and cognition (thinking). Also, the risk of physical trauma from falls during seizures may be reduced.
How to use vagus nerve stimulation
After the pulse generator is implanted, the doctor will start the stimulation, using a wand attached to a laptop computer. The doctor will begin with a low dose of current, given for 30 seconds every five minutes. The stimulation is delivered automatically, 24 hours a day. The strength of the electrical signal usually starts at 0.25 or 0.5 milliamperes (mA) and is then increased by 0.25 mA at doctor visits every few months. The frequency of the stimulation can also be adjusted to come on and off more frequently.
Your child will also be given a special magnet for use with the pulse generator. Children who experience auras (a feeling that signals the onset of a seizure) can use the magnet to give an extra burst of stimulation, which may reduce or eliminate an imminent seizure. You can also use the magnet if you see that your child is about to have a seizure. The magnet can also be used to turn off the pulse generator temporarily and to check its operation. The doctor will make sure that you and your child understand how to use the magnet before you leave the hospital.
Your child will need to continue taking their medications. The dosage will be kept constant for several months while the generator's output current is slowly increased. Once the current has been increased to its optimal level, your child's doctor will consider reducing medication and will discuss a new schedule with you.
Regular monitoring
Regular monitoring is required to check the pulse generator and battery and to make sure the treatment is working well and is not uncomfortable. The battery life of the generator is about six years, after which it may be replaced. This will require another surgery, similar to the first.
